
Journal of the Bahrain Medical Society
Year 2017, Volume 29, Issue 3, Pages 19-27
https://doi.org/10.26715/jbms.29.3.2017.39aHani Malik1*, Mohamed Ali Jaffar Ahmed Mandeel1, Ruaa Al-Zamil1, Marya Mohammed1, Amal
Dawood1, Heba Hassan1
1Department of Family Medicine, Ministry of Health—Directorate of Training, P.O Box 42, Kingdom of Bahrain.
Received date: December 25, 2016 ; Accepted date: June 21, 2017; Published date: August 22, 2017

Background and objectives: Prevalence of depression, anxiety, and stress (DAS) in primary care physicians (PCPs) have yet to be assessed in the Kingdom of Bahrain. The objectives of this study were to measure the prevalence of DAS in PCPs in the public health centers and examine the factors that influence the development of DAS.
Methods: A cross-sectional study was conducted in June 2014 using Lovibond’s short form of the Depression Anxiety Stress Scale-21, a self-report measure of DAS. A total of 336 PCPs working in the public sector at the time were identified from the Ministry of Health database and contacted to answer demographic questions included in the questionnaire.
Results: Out of 336 PCPs, 210 participated in the questionnaire with a response rate of 63%. Most of the PCPs were women (78.1%), aged between 35 and 50 years (60%), and were either family physicians or consultant family physicians. Also, 39.5% of the PCPs were found to be dissatisfied with their job. The prevalence rates of DAS were 38.6%, 37.6%, and 38.6%, respectively, ranging from mild to extremely severe. Working as nonconsultant family physicians, working for longer hours per week, dissatisfaction with the job, and taking more number of sick leaves were the risk factors for depression and/or anxiety. However, among PCPs aged less than 35 years, lower salary range and dissatisfaction with the job were the risk factors for stress.
Conclusion: The levels of mental health difficulties in PCPs cannot be ignored and need prompt action. These issues need to be addressed to provide support to PCPS and ensure the unaffected patient quality of care. Recommendations on how to improve current working conditions should be suggested to the relevant authorities.
Keywords: Depression, anxiety, stress, DASS-21, family physician, Bahrain
Introduction
Depression, anxiety, and stress (DAS) have undoubtedly been on the rise in the general population of the world. Depression is a mood disorder, which affects biological, psychological, and social function; however, anxiety is a condition with an abnormally exaggerated response and psychomotor agitation secondary to stimuli. Stress is an emotional pressure or tension suffered by a person undergoing mental and/or physical strain. With DAS, it would be interesting to see how PCPs would themselves fare against these mental health
issues.
High prevalence of DAS has been observed globally; however, there is a paucity of data on the prevalence of DAS among primary care physicians (PCPs), especially in developing countries. Few studies have been conducted in developed countries such as Netherlands, Finland, England, the United States of America, Australia, Lithuania, and Japan. In addition, few studies have also been conducted in South Africa, Tunis, Jordan, including few regional studies in the United Arab Emirates, Saudi Arabia, and Qatar.
In Netherlands, studies reported that depressive symptoms among PCPs adversely affect physicians’ attitudes towards patients and lead to medical inaccuracies.1 An extensive study in the United States of America observed substandard delivery of health care, inability of practices to retain physicians, and decreased quality of teaching when physicians were stressed or depressed.2
An Australian study examined the levels of DAS using Depression Anxiety Stress Scale (DASS- 21)score and found that 10% of the general practitioners (GP) were mildly or moderately depressed or anxious and 6% of GPs experienced severe depression and stress.3 Interestingly, 50% of the GPs at some point thought about leaving the medical profession due to stress-related reasons. Managing tasks in limited time frames and difficult patients were the highest and second highest ranking individual stress factors.3 A study in Japan observed depressive symptoms indicated in 8.3% of men and 10.5% of women, and 5.7% of men and 5.8% women exhibited suicidal ideation more than a few times during a week.4
In South Africa, a study observed high job-related stress levels among the doctors with an overall job stress index of 4.9. However, female doctors experienced greater job-related stress and lack of support on job-related stress severity than their male counterparts.5 In Tunis, professional burnout was significantly associated with depression, suicidality, and anxious temperament whereas professional exhaustion greatly impacted the relationships with patients and colleagues.6 In Jordan, a study observed the highest prevalence of stress among GPs and dentists, followed by pharmacists and specialist physicians. Stress was more pronounced in women.7 Regionally, a Saudi Arabian study observed higher suicidal tendencies and alcohol dependence among physicians than controls of a comparable social class in Saudi Arabia.8
Locally, a study examined job satisfaction at primary health centers. In a job satisfaction study in Bahrain (2008), it was observed that dissatisfied PCPs were more likely to express difficulty in caring for patients and were less able to provide quality care. In addition, they were more likely to have dissatisfied patients.9 Moreover, an earlier study in 2005 on secondary care doctors in Bahrain observed a high level of burnout with a low accomplishment rate (51.5%) and emotional exhaustion (43.1%).10
In August 2000, a study including PCPs in Bahrain concluded that physicians were stressed at work, yet were moderately satisfied. Secondary care doctors in Bahrain had a high level of burnout with a low accomplishment rate (51.5%) and emotional exhaustion (43.1%).10 Preceding the endpoint of burnout, predisposing factors need to be examined. DAS are the three of such contributing factors, which require prompt attention to prevent such catastrophic syndromes. Till date, no previous data are available about the levels of DAS in doctors of Bahrain. Thus, a cross-sectional questionnaire examining the levels in PCPs was conducted to measure the prevalence of DAS in PCPs in the local health center workplace setting and examine factors that are associated with the development of such mental illness.
Materials and methods
A cross-sectional study was conducted in June 2014 including PCPs (family physicians and GPs) working in all public sector local healthcare centers, in governorates of Bahrain. Family medicine residents currently in the training program, interns rotating in family medicine, doctors on leave at the time of data collection were excluded. The study was approved by the family practice residency program research committee.
A total of 336 PCPs were identified from a list provided from the Ministry of Health’s database of doctors. The list provided their names, designated health center, emails, and mobile or telephone numbers. The short form of Lovibond’s (1995) 42- item self-report measure of depression, anxiety, and stress scale (DASS-21) was used.11 DASS-21 has been reported to have an internal consistency of >80% across all three domains.12 Demographic personal data including gender, nationality, marital status, and medical illness were also collected, along with work-related details.
Procedure and data collection
Data collection was assorted into three phases for 7 weeks. During phase I, SurveyMonkey was used. The questionnaire was entered into SurveyMonkey, and subsequently emailed to the PCPs. PCPs were assured about confidentiality through these emails as well. Four weeks were allocated in this phase, during which reminder emails were regularly sent to the doctors who were yet to answer the questionnaire. Once the response rate started to lag, phase II was started.
During phase II, mobile phone text messages were sent to PCPs who were yet to answer the questionnaire. The messages contained a web link to the questionnaire via SurveyMonkey, as well as assurance of confidentiality. Two weeks were allocated to this part of the data collection, where reminder texts were sent at regular intervals. Again, once the response rate started to lag again, phase III was initiated.
During phase III, local healthcare centers with the lowest number of responders were identified and visited, and physical copies of the questionnaire and sealable envelopes were handed out to the PCPs. The PCPs were asked to answer the questionnaire anonymously, place and seal it in the envelope, and return it to the data collectors. To ensure confidentiality, two of the researchers who were not involved in data collection were made responsible for manually entering the data into SurveyMonkey ensuring answers were not traceable to the responders during this final phase. Data were exported from SurveyMonkey and analyzed with IBM statistical package for social sciences (SPSS) version-20. Logistic regression analysis was used to assess the risk of developing either depression, anxiety, or stress in relation to personal and workrelated parameters.
Results
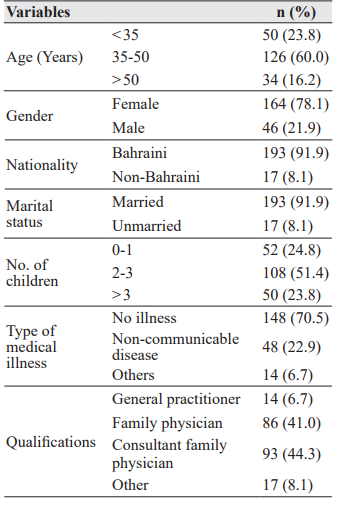
Out of 336 total PCPs in the study population, 210 participated in answering the questionnaire with a response rate of 63%. The participants were predominantly women (78.1%) and Bahraini (91.9%; Table 1). Most of the PCPs (60%) were in the age-group of 35-50 years with a mean age of 41.7±8.7 years, and not suffering from any illness (70.5%). The majority of the PCPs were either family physicians (41%) or consultant family physicians (44.3%).
Table 1: Personal data of primary care physicians in Bahrain (N=210)
Work-related data among the population is represented in Table 2. For salary range, most of the respondents fell into the range of 1200-1600 Bahraini Dinar (BD; 40.5%), while the rest were distributed across the highest pay range. Most PCPs (64.6%) were observed to have working hours of approximately 40-50 h per week, which included the duties/calls per month. Also, 78.3% of the PCPs worked approximately 5-10 duties/calls per month. PCPs were mostly seeing approximately 200-350 (63.4%) patients per week; however, 20% were consulting more than 350 patients. In terms of overall satisfaction, 39.5% of PCPs answered “No” when asked about job satisfaction. Also, 98.1% of PCPs were full-time employees. Work-related data among the population is shown in Table 2.
Table 2: Work-related data of primary care physicians in Bahrain (N=210)
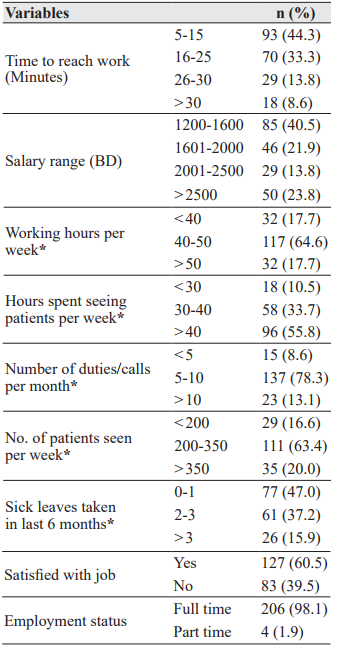
*Variables had missing data due to parameters unanswered
by some participants BD - Bahraini Dinar
Depression, anxiety, or stress levels
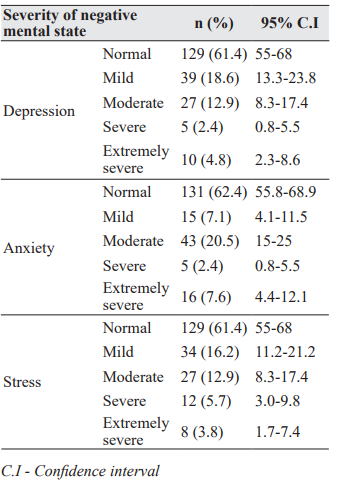
The levels of DAS in the participants ranged from mild to severe (Table 3). The mean scores for the DAS were 8.9±8.1, 7.1±7.0, and 13.7±8.6, respectively. In this study, 38.6% of the PCPs had depression, in which 18.6% of PCPs had mild depression and 12.9% suffered from moderate depression. Also, 37.6% of PCPs had anxiety, of which, most suffered from moderate levels (20.5%). Similarly, 38.6% of PCPs were found to be stressed and most were suffering from either mild (16.2%) or moderate (12.9%) stress.
Table 3: DASS severity of primary care physicians in Bahrain. (N=210)
Depression
Family physicians were found to be 4.5 times more likely to be depressed than consultant family physicians (P=0.001; Table 4). Age-group (35- 50 years; P=0.84), marital status (unmarried, P=0.111), and gender (male doctors; P=0.347) were also the factors for depression; however, these were not statistically significant.
As represented in Table 5, PCPs with salaries ranging from 1200 to 1600 BD were four times more likely to be depressed than those earning more than 2500 BD (P=0.032). Also, PCPs who worked for <40 h per week were 14.3 times more likely to be depressed than those who worked for >50 h per week (P=0.019). Whereas, PCPs who spent 30- 40 h (P=0.016) consulting patients per week were 13.1 times more likely to be depressed compared to those who spent < 30 h per week. With regards to patient load, PCPs who consulted < 200 patients per week were 33.3 times and 27 times more likely to be depressed compared to those who consulted 200-350 patients (P=0.001) and > 350 patients per week (P=0.008), respectively.
Table 4: Odds ratio for depression, anxiety, & stress with personal data
PCPs who took more than 3 days of sick leaves (P=0.011) in the past 6 months were 7.2 times more likely to suffer from depression than those who took 0-1 days leave during the same period. Finally, PCPs who answered “No” (P<0.001) when asked about job satisfaction were 12 times more likely to be depressed compared to their satisfied colleagues. Despite being statistically insignificant, PCPs with factors such as taking > 30 min to reach work place (P=0.105) were found more likely to exhibit depression.
Anxiety
Family physicians were 8.6 times and 5 times more likely to suffer from anxiety than GPs (P=0.020) and consultant family physicians (P<0.001), respectively (Table 4). Despite being statistically insignificant, factors like being non-Bahraini (P=0.402), unmarried (P=0.309), and suffering from other medical illnesses (P=0.121) were found more likely to exhibit anxiety.
PCPs who answered “No” (P=0.001) when asked about job satisfaction were 5.1 times more likely to suffer from anxiety than those considered to be satisfied (Table 5). Despite being statistically insignificant, doctors, who did more than 10 duties/calls per month (P=0.322), spent > 40 h for consulting patient per week (P=0.442), and took > 3 sick leaves in past 6 months (P=0.057) were found more likely to exhibit anxiety.
Stress
PCPs aged <35 years were 9.9 times more likely to be stressed in comparison to doctors older than 50 years (P=0.016), as shown in Table 4. Also, family physicians were 3 times more likely to be stressed than consultant family physicians (P=0.013). Despite being statistically insignificant, factors such as being non-Bahraini (P=0.350), unmarried (P=0.054), and suffering from other medical illness (P=0.056) were found more likely to exhibit stress.
Table 5: Odds ratio for depression, anxiety, & stress with work-related data
As represented in Table 5, PCPs with a salary ranging from 1200-1600 BD were 5.4 times more likely to be stressed than those who earned more than 2500 BD (P=0.011). Finally, those who answered “No” (P<0.001) when asked about job satisfaction were 28.1 times more likely to be stressed than those who answered “Yes”. Despite being statistically insignificant, PCPs who took > 30 min to reach work place (P=0.227), spent 30-40 h for consulting patients per week (P=0.161), and took > 3 sick leaves in past 6 months (P=0.077) were found more likely to exhibit stress.
Discussion
Prevalence rates of 38.6%, 37.6%, and 38.6% for depression, anxiety, and stress, respectively in PCPs were high when compared to studies conducted elsewhere. An Australian study that used DASS- 21 reported 10% of GPs in the study were mildly or moderately depressed or anxious and 6% experienced severe depression and stress.3 While a study in Saudi Arabia had prevalence rates of 7.6 %, 8.6%, and 7.2% for depression, anxiety, and stress, respectively for their PCPs.8 Regionally, a study conducted in Dubai observed results similar to that of Saudi Arabia, where 7.8% of medical staff showed depression and 2.2% of them showed anxiety. However, 2.6% of the medical staff was moderately depressed.13 This could be due to a different system, remuneration, and more reasonable working hours and patient load. However, the results did compare to some studies from the literature. A study in Netherlands including 423 physicians reported 29% of physicians with depression, 24% with anxiety, 15% with post-traumatic stress disorder and stress, and 6% with burnout.1 Also, a study in Lithuania found that 48% of respondents could be classified as suffering from work-related psychosocial stress.14
The current study found the most of the PCPs were women, which has been a trend in Bahrain since the conception of family medicine residency program. From experience, male doctors are drawn more toward secondary care specialties. Most studies in the literature review discussed higher levels of DAS with relation to gender. For example in Saudi Arabia, anxiety and stress were significantly higher among female physicians than male physicians (15.5% vs. 6.9%, respectively, P=0.035 for anxiety; and 13.8% vs. 5.7% for stress, respectively, P=0.032).8 On the contrary, an English study found that male GPs exhibited higher levels of free-floating anxiety and depression and lower levels of somatic anxiety, while scores for female GPs on somatic anxiety and depression were lower than the norm.15 However, in this study, there was no clinical significance with regards to the gender difference in DAS levels.
Younger PCPs were nine times more likely to be stressed than their older counterparts. This could be due to less work experience coupled with a higher patient load. In addition, family physicians were seen to be more depressed, susceptible to anxiety, and stressed than consultants and GPs. This could also be attributed to less work experience and more patient load for family physicians compared to consultants. In comparison to a study in Finland, age and length of service had important influence in the level of stress and burnout syndrome: the older the physicians and the higher the length of service, the higher the level of stress and the higher the risk of burnout syndrome.16
Working hours and patient load were one of the alarming results, which need further review. It is worth noting that primary care is legislated by the government, easily accessible, and carries no financial burden on Bahraini citizens who attend. The Ministry of Health has designated 8 min per patient consultation in the health center. Doctors were mostly consulting with 200–350 (63.4%) patients per week; however, 20% were seeing more than 350 patients per week. This is quite a large number of patients, which roughly translates to approximately 40-70 patients per day. Since each working day is 7-h long, with half an hour break, if a doctor sees 350 patients per week, simple calculation equates this to approximately 5.6 min per each patient. This clearly is not enough time to adequately evaluate and manage patients. Furthermore, doctors also consult walk-in patients, which put a further load on the already congested patient list. Consequently, doctors are not able to predict how many patients in total they will actually consult, and in fear of not finishing on time, they, unfortunately, tend to rush through consultations to equate for this. In addition, 78.3% of the doctors work approximately 5-10 duties/calls per month. These duties were evening shifts of 4 h. They carry the same number of the patient load as a regular shift, and at times doctors have 6 min allocated per patients, especially on public holidays. In a Qatar study, 80% of the doctors agreed that there was insufficient time to do justice to the patients during consultations and incidentally, there was more stress in women than in men and more stress in Qatari than non-Qatari doctors.17
PCPs were found to be more depressed and stressed when their salary is in the lower bracket. This correlation would be expected, especially the obligations PCPs have. Approximately, 75.2% of PCPs have 2-3 or more children, and they would likely not be satisfied with a lower salary bracket. Also, PCPs who took more than 3 days of sick leave in the past 6 months were observed to be 7.2 times more depressed than those who took ≤1 day sick leave. It could perhaps be indicative of possible underlying negative emotional states.
PCPs who consulted less than 200 patients were seen to be more depressed than those who consulted 200-350 and more than 350 patients per week. Also, PCPs who worked less than 40 h per week were seen to be more depressed than those who worked more than 50 h per week. These unexpected results could be attributed to certain health centers in Bahrain including Al-Razi health center where doctors generally had a more positive and obliging disposition as found during phase III of the methodology. Despite seeing a large number of patients and spending more hours working per week, the doctors at Al-Razi health center verbally expressed satisfaction with their work environment and circumstances. The demographics of the patients who attended Al-Razi health center were mainly labor workers from South-east Asia who were quite cooperative and accepting of doctor’s decision with no incident, despite the language barrier. As a result, PCPs working at health centers such as Al-Razi are quite happy to see a larger number of patients, potentially being the reason for the results. In terms of overall satisfaction, 39.5% of the PCPs were not satisfied with their job. This was a significantly high number, especially the doctors who were not satisfied were 12 times more likely to be depressed, 5.1 times more likely to suffer from anxiety, and 28 times more likely to be stressed.
Strengths
This study used an internationally validated questionnaire, with favorable Cronbach’s Alpha scores. The DASS questionnaire in this study overall showed a Cronbach’s Alpha of 0.936. The DAS subscales had a Cronbach’s Alpha of 0.879, 0.831, and 0.873, respectively. The study also boasts a 63% respondent rate where the population group of PCPs in the public sector was taken in its entirety.
Limitations
This study might have been biased, as some PCPs were made to answer under duress, specifically due to time constraints. Also, the study might have a limitation since the obtained data were selfreported, hence, some degree of response bias due to under-reporting might have occurred. Some of the PCPs did not do the same amount of work and did not consult the same number of patients adding to selection bias. There were other confounding factors, which were not kept in consideration, for example, most of the PCPs were women in the study and women being more prone to mental illness compared to men.
Conclusion
Mental health difficulties were alarmingly high in PCPs. Younger PCPs, nonconsultant family physicians, longer working hours per week, and lower salary brackets were found to be the risk factors for developing mental illness. Dissatisfaction with the job (39.5% of the PCPs) was the common cause of DAS in PCPs. In addition, those who took more sick leaves than their colleagues were also more likely to be depressed. These results cannot be ignored, as the patient welfare and care would possibly be at risk.
Recommendations
Intervention is promptly required for PCPs, where full assessment, support, and therapy needs to be provided for current sufferers of DAS. Increasing allocated time per patient during consultation could be a solution to ensure adequate care was provided. Also, a higher salary bracket could act as an incentive for doctors, who are increasingly dissatisfied with their jobs. Improving public education and community awareness could also decrease the burden on health centers and their doctors.
Further research in this field is warranted, as high levels of burnout were found in secondary care doctors in a study in Bahrain conducted in 2005. We predict that the levels of DAS would probably be significant in that study population as well. Based on the findings of this study, these issues are needed to be adequately addressed so it does not negatively impact the quality of patient care, and prevent any chances of an exodus of PCPs from the public sector to private practices and other departments/ branches.
1. Ruitenburg MM, Frings-Dresen MH, Sluiter JK. The prevalence of common mental disorders among hospital physicians and their association with self-reported work ability: A cross-sectional study. BMC Health Serv Res. 2012;12(1):292.
2. Costa AJ, Schrop SL, McCord G, et al. Depression in family medicine faculty. Fam Med. 2005;37(4):271-5.
3. Schattner P, Mazalin D, Pier C, et al. GP registrar well-being: A cross-sectional survey. Asia Pac Fam Med. 2010;9(1):2.
4. Wada K, Yoshikawa T, Goto T, et al. Association of depression and suicidal ideation with unreasonable patient demands and complaints among Japanese physicians: A national cross-sectional survey. Int J Behav Med. 2011;18(4):384-90. 27 Malik et al., J Bahrain Med Soc. 2017;0(3):19-27
5. Govender I, Joubert G, Oosthuizen SD. Stress among general practitioners of Kwa-Dukuza, Kwa-Zulu Natal. Afr J Prim Health Care Fam Med. 2009;1(1):1-4.
6. Oumaya M, Ghanmi L, Baccar Y, et al. P03-259 burnout or professional exhaustion syndrome among primary care Tunisian doctors. Eur Psychiatry. 2009;24:258.
7.. Boran A, Shawaheen M, Khader Y, et al. Workrelated stress among health professionals in northern Jordan. Occ Med. 2011;62(2):145-7.
8. Khalid S. Al-Gelban YMA-K, Hasan S. AlAmri, Ossama A. Mostafa. Emotional status of primary health care physicians in Saudi Arabia. Middle East J Fam Med. 2009;7(5):3-7.
9. Sharaf E, Madan N, Sharaf A. Physician job satisfaction in primary care. BMB. 2008;30(2):43-52.
10. Hasan HI, Nooh Y, Alsayyad AS. Prevalence and factors affecting burnout among secondary care doctors in Bahrain-a cross sectional study. IJMRHS. 2015;4(2):401-6.
11. Lovibond P, Lovibond. Manual for the depression anxiety stress scales. The Psychology Foundation of Australia Inc. 1995.
12. Henry JD, Crawford JR. The short-form version of the depression anxiety stress scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44(2):227-39.
13. Ahmed I, Banu H, Al-Fageer R, et al. Cognitive emotions: Depression and anxiety in medical students and staff. Crit Care. 2009;24(3):1-7.
14. Vanagas G, Bihari-Axelsson S. The factors associated to psychosocial stress among general practitioners in Lithuania. Cross-sectional study. BMC Health Serv Res. 2005;5(1):45.
15. Rout U. Gender differences in stress, satisfaction and mental wellbeing among general practitioners in England. Psychol Health Med. 1999;4(4):345-54.
16. Kuusio H, Heponiemi T, Aalto AM, et al. Differences in Well-being between GPs, medical specialists, and private physicians: The role of psychosocial factors. Health Serv Res. 2012;47:68-85.
17. Alkhalaf JH, Singh R, Malallah M, et al. Job satisfaction and stress level of primary health caregivers at primary health centers in Qatar. Int J Med. 2009;2(2):245-50.