
Journal of the Bahrain Medical Society
Year 2018, Volume 30, Issue 2, Pages 38-46
https://doi.org/10.26715/jbms.2_13082018Waiel Hikmet Salman Alani1, Mohamed Ahmed Serageldein2*, Wafa Khalid Almutawaa3, Haya Mohamad Al-Noaimi4, Zain Jassim Buallay5
1Consultant Psychiatrist, Bahrain Defense Force Hospital, Kingdom of Bahrain.
2Senior Psychiatric Resident, Department of Psychiatry, Bahrain Defense Force Hospital, Kingdom of Bahrain.
3Psychiatric Resident, Bahrain Defense Hospital, Kingdom of Bahrain.
4Psychiatric Resident, Bahrain Defense Hospital, Kingdom of Bahrain.
5Psychologist, Bahrain Defense Hospital, Kingdom of Bahrain.
*Corresponding author:
Mohamed Serageldein, Senior Psychiatric Resident, Department of Psychiatry, Bahrain Defense Force Hospital, Kingdom of Bahrain; Tel: (+973) 34135982, Email: mserag5414@gmail.com
Received date: July 30, 2018; Accepted date: August 16, 2018; Published date: September 21, 2018

Background and objectives: According to the WHO Global Burden of Disease, the lifetime prevalence of major depressive disorder (MDD) is about 15%. Most of the MDD patients ranging between 18–45 years cause economic and social burden on the families and the country as a whole. The objective was to assess the quality of life (QoL) of patients with depression and to evaluate whether the impairment of QoL is specific for MDD or it is a general phenomenon.
Methods: The case–control cross-sectional study, including 30 patients aged between 18 and 45 years fulfilling the criteria of MDD according to the Diagnostic and Statistical Manual of Mental Disorders–4th ed., were recruited from the outpatient psychiatric clinics at the Bahrain Defense Force (BDF) Hospital. The case group was compared with age- and sex-matched control group, including 20 healthy volunteers selected among employees of the BDF Hospital. All patients underwent (a) general medical and neurological examinations, (b) a Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders–4th ed., Axis-I (SCID-I), (c) 17-item Hamilton Depression Rating Scale (HAMD-17), and (d) Short-Form 36 Health Survey Arabic Version 1.0 (SF-36). The control group was subjected to a physical examination, SCID-I (nonpatient version). Statistical analysis of the data was conducted.
Results: The educational level (P < 0.001) and the types of employment (P = 0.002) were statistically significant when compared between cases and controls. In the case group, quality of life as greatly affected by the severity of MDD with marked impairment in the social function and the overall mental function (P < 0.001). A significant decrease was observed in the physical function (P < 0.001) and vitality (P = 0.010) of the cases when compared to their healthy counterparts. A high statistical difference (P < 0.001) between the cases and controls was observed with respect to the eight domains of the QoL scale.
Conclusion: Depression has a markedly significant impact on the QoL of MDD patients. There is a marked reduction in functioning of patients who suffer from depression in comparison to the nondepressed population.
Keywords: Severity of depression, major depressive disorder, Quality of life related health, Short form-36, physical component scale, mental component scale
Major depressive disorder (MDD) is a common illness associated with relatively long duration of episodes, high rates of chronicity, relapses, and recurrence. Depressive disorders are highly prevalent and are associated with functional, psychological, and occupational impairment.1 According to the World Health Organization, the burden of depression is ranked 4th among disabling diseases and is projected to increase to 2nd position in 2020.2
MDD is one of the most common mental illnesses and is regarded as a major public health problem, worldwide. In the United States of America, the National Comorbidity Survey Replication (NCS-R) showed that the lifetime and 12-month prevalence of MDD were 16.2% and 6.6%, respectively. According to the World Health Organization (WHO), the lifetime risk of MDD among men and women were 7–12% and 20–25%, respectively.3 An epidemiological survey of the four provinces in China showed that the prevalence of major depressive disorder among the general population was 2.07%.4 He et al.5 found that the prevalence of depression in general hospitals was as high as 12.1%.
Recent studies report 4.1% and 6.7% 12-month prevalence rates of MDD among Australians and Americans, respectively.3 The prevalence of MDD in Bahrain is projected to be 5.6% according to a study conducted in the four Governorates.6 According to literature, patients with depression experience physical, psychological, and social problems as well as decline in health-related quality of life (QoL). Further, increased financial pressure, social and family relationship issues, occupational dysfunction, increased days of absence from work, and poor health status have been reported as well.7
QoL is a multi-dimensional concept, which is used to describe the individual’s perceptions, satisfaction, and evaluation of different areas of their own lives, such as physical health and functioning, psychological and emotional well-being, social roles and relationships. Extensive research has not been conducted regarding the QoL in individuals with depression versus healthy subjects. The complex subjective and dynamic nature of the concept of QoL presents methodological challenges to its measurement and interpretation.8 However, several epidemiological investigations indicate that individuals suffering from depression are subject to impoverished external living conditions. According to National Institute of Mental Health (NIMH) Epidemiological Catchment Area Program, patients with MDD or subsyndromal depression experience higher levels of household strain, social irritability, financial stress, limitation in occupational functioning, poor health status, and days lost from work. Another study also found that women with major depressive disorder had impairment in family, marital, occupational and leisure activities. Depressive disorders have impacted negatively on the QoL of patients.3
Depression scales, such as 17-item Hamilton Depression Rating Scale (HAMD-17) do not include important domains of QoL.9 Therefore, a Short-Form 36 Health Survey Version 1.0 (SF-36), which is a multipurpose health survey has been used to measure the overall health status, functional status, and health-related QoL. SF-36 is a generic measure and its use is not restricted to a single disease state. The SF-36 is a valid and reliable tool that allows comparisons between and within the clinical and general population. An eight-scale profile of physical and mental health measures as administered, including Physical Functioning (PF), Role Physical (RP), Bodily Pain (BP), General Health Perceptions (GH), Vitality (VT), Social Functioning (SF), Role Emotional (RE), and Mental Health (MH).
Despite the debilitating nature of depression, about 50–60% of cases remain undetected in the primary care and the diagnosed patients do not receive appropriate and specific treatment.10 Numerous studies have been conducted in western countries regarding the QoL among patients with depression, while there have been few studies conducted in the eastern countries.7 Hence, the present study was conducted to evaluate QoL in MDD patients to offer better understanding of psychosocial impact of MDD. The objective was to assess the quality of life of patients with depression and to evaluate whether the impairment of quality of life is specific for MDD or it is a general phenomenon.
A case–control cross-sectional study, including 30 participants aged 18–45 years and who met the diagnostic criteria of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) for depression and were capable and willing to complete the QoL questionnaire during the study period—January 2016 and August 2017—were recruited from the outpatient psychiatric clinics of Bahrain Defense Force (BDF) Hospital. Participants with concurrent medical condition and any other psychiatric disorder were excluded from the study.11 Healthy age- and sex-matched control volunteers among the employees of BDF Hospital were included as a control group.
Ethical approval was obtained from the Research and Ethics Committee BDF Royal Medical Services. A written informed consent was obtained from the participants before commencing the study. Participants were adequately counseled before the interview to anticipate the possibility of traumatic memories (relapse) or discomfort.
The participants were invited to complete the questionnaires concerning QoL and related clinical information at their visits. The contents of the questionnaire included information on demographics, QoL, general health, and severity of depression. The Arabic version proved valid and reliable through different studies,12-15 was employed.
Cases of the study were administered the following questionnaires:
a. General medical and neurological examination
b. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I): performed by the researcher in private setting for Diagnosis of MDD.
c. HAMD-17: clinician administered depression assessment severity scale.16
d. SF-36 Arabic Version 1.0.12
The control group participants were subjected to physical examination, SCID-I (nonpatient version), and SF-36.
Variables of the participants including sex, age, occupation, and education were recorded.
Quality of life—36-item Short Form Health Survey Arabic Version 1.0 (SF-36)
The 36-item Short Form Health Survey Arabic Version 1.0 (SF-36) is one of the generic QoL tools as reported in many studies.12-15, 17 It can be used in clinical practice and research to evaluate, follow, and supervise population health status, estimate the burden of different diseases, monitor outcomes in clinical practice, and evaluate treatment effects. It has high standard of reliability, validity, and good sensitivity to change in health status.
The SF-36 is a brief self-administered questionnaire based on 35 items divided into 8 health domains: physical function (PF: 10 items), role limitations caused by physical health functioning (RP: 4 items), role limitations caused by emotional problems (RE: 3 items), social functioning (SF: 2 items), mental health (MH: 5 items), vitality (VT: 4 items), bodily pain (BP: 2 items), and general health perception (GH: 5 items). Two summary scores were calculated from the 8 domain scores, which include a physical component score (PCS) that include PF, RP, BP, and GH and mental component score (MCS) that include VT, SF, RE, and MH. Item number 36 is a general question on health transition and is not calculated in the summary scores. The scores are interpreted from 0 to 100, with lower score indicating lower level of function and/or bad health and higher score indicating higher level of function and/or better health.18
Depression severity—17-item Hamilton Depression Rating Scale (HAMD-17)
The HAMD-17, also known as HDRS or Ham-D is a scale to determine the patient’s level of depression. It has a list of 21 symptom-oriented questions. The scoring is based on the first 17 questions only. Nine of the items are scored on a five-point scale, ranging from zero to four. The scores indicate: 0, absence of the depressive symptom being measured; 1, doubt concerning the presence of the symptom; 2, mild symptoms; 3, moderate symptoms; and 4, presence of severe symptoms. The remaining eight items are scored on a three-point scale, from zero to two. The scores indicate: 0, absence of symptom; 1, doubt that the symptom is present; and 2, clear presence of symptoms. Based on the total score, a score of 0–7 indicates no depression, 8–16 mild depression, 17–23 moderate depression, and ≥ 24 severe depression.16
The data were analyzed using Statistical Package for Social Science version 15 (SPSS Inc., Chicago, Illinois, USA). The socio-demographic variables, QoL for both cases and controls, and correlation between severity of depression and QoL were analyzed. Categorical data were summarized as frequency and percentages; continuous data were summarized as the mean and standard deviation. Chi-square test or Fisher’s exact test were used to compare the categorical variables, as appropriate. Independent t-tests were conducted for betweengroup comparisons of quantitative variables and One-way ANOVA was employed for more than two group comparisons. Pearson’s correlation was used to determine correlation between the variables.
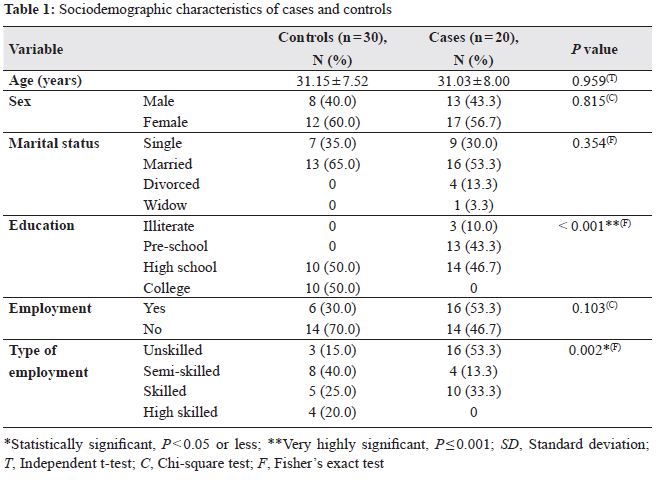
The case group included 30 patients with a mean age of 31.03 ± 8 years while the control group comprised of 20 participants with a mean age of 31.15 ± 7.52 years. Most of the subjects were females (58%) and married 16 (53.3%). In terms of employment, 16 (53.3%) individuals were not employed, while 14 (46.7%) were employed. There was no significant difference between these variables of cases when compared to the control group. However, most of the patients in the case 14 (46.7%) and control 10 (50%) group were graduates from the high school with a high statistically significant difference (P < 0.001). In terms of the types of employment, most of the patients were unskilled in the case group when compared to the control group (16, 53.3% vs. 3, 15%; P = 0.002; Table 1).
Quality of life and its correlation to MDD severity and demographic data
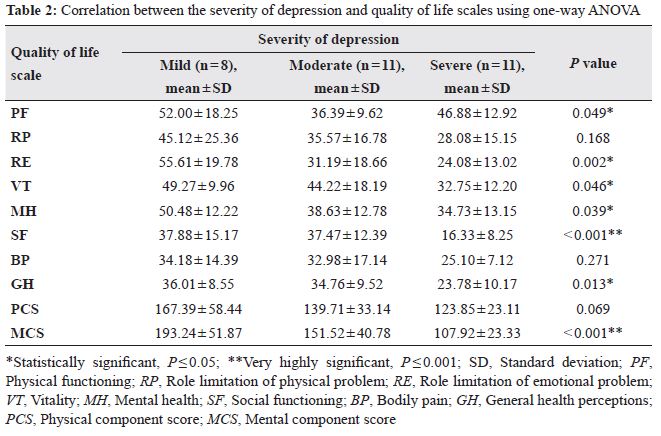
Regarding the effect of severity of depression on SF-36 subscales, cases were found to have a very high statistically significant difference (P < 0.001) in social functioning (SF) and mental component score (MCS). While role limitation of emotional problems shows a high statistically significant difference (P < 0.002). Further, there was statistically significant difference between SF-36 score and severity of depression scores of HAMD-17 scale of the cases: PF (P = 0.049), VT (P = 0.046), MH (P = 0.039), and GH (P = 0.013; Table 2). However, the correlation between the severity of depression and QoL scale regarding role limitation of physical problems (RP), body pain (BP), and physical component score (PCS) showed no statistical significance.
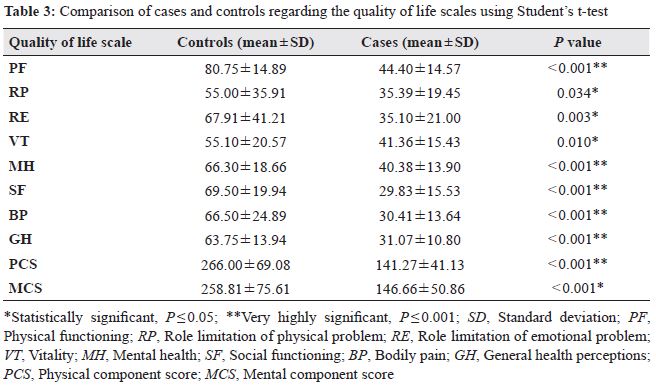
Moreover, all SF-36 domains were significantly different between both groups. As shown in Table 3, it was observed that PF, MH, SF, BP, GH, PCS, and MCS were very highly statistically significant (P < 0.001), while RE (P = 0.003), RP (P = 0.034), and VT (P = 0.010) showed a high statistically significant difference.
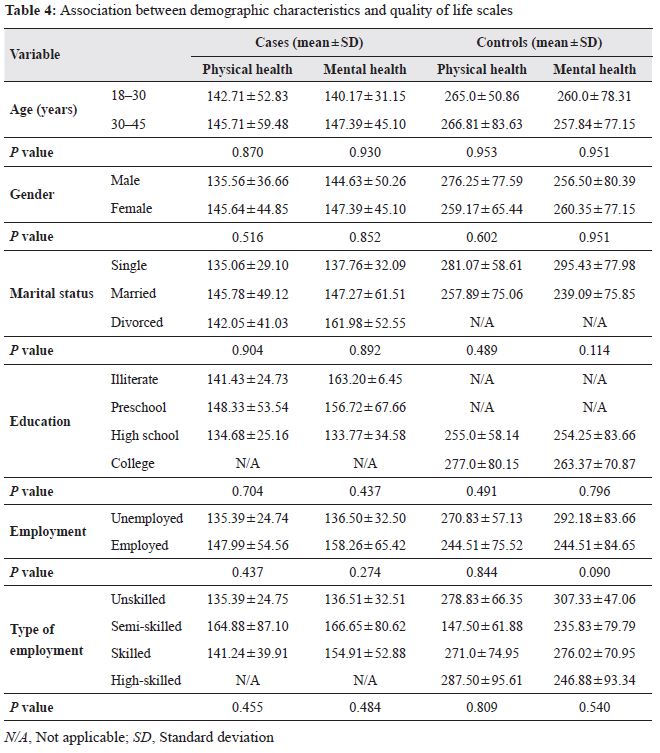
Statistically significant difference was not observed between the cases and controls regarding the effect of demographic characteristics on QoL scales in relation to the SF-36 domains (Table 4).
Depression interferes with the individual’s ability to fulfill their needs and adapt to the setting, which have a negative impact on the QoL. Adequate treatment of depressive symptoms improves the subject’s ability to reach and fulfill personal needs, which leads to improvement in the quality of life-related health (QLRH). Our study intended to investigate the correlations between MDD and the impairment of daily life properties. Self-evaluation scales were applied that have been used and validated in various studies12-15, 17 and settings.
Sociodemographic features of participants
A female preponderance was observed in the cases and controls under study. This conforms to the findings of Rocha et al.19 who evaluated and validated the World Health Organization Quality of Life questionnaire (WHOQOL-BREF) in depressed Brazilians and reported a female dominance 156 (75.0%) among the study subjects. FJ Davou et al.1 observed that females constituted the majority of participants among cases (64.0%) and controls (60.0%), while studying the subjective QoL in outpatients with depression.
The preponderance of females in our study is consistent with the WHO epidemiological results indicating that more women suffer from depression than men. This might be attributed to the periodic fluctuation of female hormones, which reinforce the physical stress-response that may amplify vulnerability to depression. Moreover, men with alcohol and substance abuse comorbidity were excluded from the study.
Most of the study subjects had secondary education, while no one accomplished graduate level education. In a study conducted by Davou et al.,1 18.0% participants were illiterate, 15.5% had acquired primary education, while 38.5% had secondary education. Similarly, Afolabi et al.11 reported 21.6% illiterates and 21.2% primary and secondary education participants each. In addition, they observed that lower level of education is strongly linked with the risk of depression. Due to the cultural bias, most parents do not send their children, especially girls, to school and prefer to marry them out as teenagers. Further, another leading cause of low enrolment is that many families cannot afford the expenses educating their children. In our study a high rate of lack of education is expected due to these reasons.
In contrary to the controls, most of the cases in the study were unemployed. The low employment level among the cases could be due to the discrimination and stigma around depression leading to job loss or outright refusal to employ individuals with mental illnesses, despite their qualifications. This low employment status leads to lack of financial independence, which is known to improve selfesteem and reduce stress. In contrary to our study, Agbir et al.,20 while determining the prevalence of depression among medical outpatients with diabetes observed that majority of the subjects were employed, while a quarter of them were not.
Comparison of domain scores
In our study, a statistically significant correlation was observed between the cases and controls regarding the eight QoL domains. A comparative analysis of the mean scores revealed that depressed cases scored lower than the control group, which is suggestive of poor QoL. This was consistent with the studies conducted by Yen et al. and Amini et al., 21, 22 who stated that depressive subjects had poor QoL on the physical, psychological, and social relationship domains than the non-depressive control group. Similarly, Davou et al.1 reported a negative association between the QoL domains and depressive disorder, indicating depression significantly lowered QoL in the respective domains.
The findings of Xia et al.23 conformed with our study, wherein, the scores of the QoL domains were significantly lower than the average scores of the cases from the large community surveys in the populations of Guang Zhou. Zikic et al.24 also, found that, the score for the domains of QoL reported in 84 patients with depression was significantly lower than the score reported by 30 normal subjects in a study aiming to investigate the relationship between unipolar depression and QoL.
The overall physical health domain, which assesses areas such as pain, fatigue, vitality, and sleep was impaired among the cases as they scored poor on the SF-36. This can be explained by the fact that depression, as an illness, reflects negatively on the energy levels, sleep, and pain. Chin et al.25 reported a statistical significance regarding the physical health items (PF, RP, BP, GH) wherein PF had shown a statistically significant difference together with continuous sense of fatigue with RP (P =0.034). On the other hand, in our study, mental health domains have shown a significant difference between the cases and control. Likewise, in a study conducted by Chin et al.25 the depressed cases rated worse QoL than the control group. This might be due to the fact that depression, as a clinical entity, is always associated with negative cognition and negative self-perception.
Among a number of factors that affect the QoL of the individuals with depression, the severity of depressive symptoms is one of the important determinants. In our study, it was obvious from the results that there is an inversely proportional relationship between the severity of depression and the QoL domain scores. This is in accordance with the study conducted by Chung et al.26 among depressed patients in Taiwan, wherein, the severity of depressive symptoms and social isolation were reported to have a direct effect on all domains of QoL. Further, Jung et al.27 observed that more severe the depressive symptoms, poorer the QoL. In contrary, Nuevo et al.28 observed no significant relationship between QoL and the severity of depressive symptoms. However, they believe that the significant relationships were distorted by the inappropriate severity grading of the ICD-10.
Individuals with major depression have a substantially decreased subjective QoL than those without depression or healthy subjects. Depression has a markedly significant impact on the QoL of the patients with depression. Subjective assessment of the QoL domains revealed poor QoL among the cases when compared to the controls. There is a marked reduction in functioning of the patients with MDD in comparison to the nondepressed population. Treatment programs need to be developed to improve the screening of the depressive symptoms, which will improve the QoL outcome in the patients with depression.
Several limitations have to be considered in this exploratory study, including small sample size, contrast between the non-significant statistical results, which may be explained due to the lack of power, and the small to moderate level of effect sizes.
The authors would like to thank the BDF Hospital for facilitating the requirements for this research. Further, we want to thank Fatima Al Atawi (Psychiatric nurse) for her cooperation and all those patients who participated in the study, despite their time constraints.
WA and MS shared in the choice of the study subject, designed the study, and wrote the protocol. WM, HN, and ZB helped in conducting the assessments and questionnaires. MS managed the literature searches, statistical analysis as well as the final manuscript. All authors approved the final manuscript.
The authors of the study have no conflict of interest to declare.