
Journal of the Bahrain Medical Society
Year 2019, Volume 31, Issue 1, Pages 30-36
https://doi.org/10.26715/jbms.2019.1_20032019Samir Selimi1 , Gazmend Spahija2 , Lul Raka3, 4*
1London School of Hygiene & Tropical Medicine, London, United Kingdom.
2 Department of Intensive Care, University Clinical Centre of Kosovo, Prishtina, Kosovo.
3 University of Prishtina “Hasan Prishtina”
4 National Institute of Public Health of Kosovo, Prishtina, Kosovo.
*Corresponding author:
Lul Raka, University of Prishtina “Hasan Prishtina” and National Institute of Public Health of Kosovo, Prishtina, Kosovo, Tel: +38344368289, Email: lul.raka@uni-pr.edu
Received date: December 30, 2018; Accepted date: March 20, 2019; Published date: March 31, 2019

Background and objective: Ventilator-associated pneumonia (VAP) is a predominant type of healthcareassociated infection (HAI) in intensive care units (ICU), associated with increased length of stay(LOS), mortality rates, and costs. We aimed to assess the financial burden of VAP in terms of direct medical costs incurred by the patients treated in ICU.
Methods: A local surveillance dataset was used to perform the assessment of direct medical costs incurred by the patients while being treated for VAP in the ICU at University Clinical Centre of Kosovo (UCCK).
Results: Overall, incidence rate of HAIs in the ICU at UCCK was 62.1% with VAP dominating the infection account (73.2%). The LOS in ICU ranged from 2–44 days with a median time of six days, while the distribution between VAP affected and unaffected patients ranged between 13.5 and 5.4 days, respectively. The mean cost to patients with VAP is estimated as €647±487, which is significantly higher than in patients without VAP (€227±174).
Conclusion: An immediate action is required to introduce better VAP prevention and control measures in the ICU. Evidence-based practices confirm that compliance to hand-hygiene practices, ICU staff education, introduction of regular surveillance, and adequate antibiotic therapy can significantly decrease VAP incidence, save lives, decrease LOS, and reduce costs.
Keywords: Costs, intensive care unit, Kosovo, ventilator-associated pneumonia
Worldwide, healthcare-associated infections (HAIs) constitute a major public health concern. They result in high morbidity and mortality, prolonged hospital stay, and increased costs.1-3 The European Centre for Disease Prevention and Control (ECDC) reports that over four million patients are affected by HAIs every year in Europe with a mean prevalence of 7.1% resulting in approximately 37,000 deaths as a direct consequence of the infection.4 The HAIs cause 16 million extra-days of hospital stay and the annual financial losses are estimated at approximately €7 billion.4
Ventilator- associated pneumoniae (VAP) is the most frequent HAI in intensive care units (ICU) and is associated with increased ICU and hospital length of stay (LOS) and elevated costs and mortality rates.5 The mechanical ventilation is a primary risk factor in the development of VAP and its incidence is 3–10 fold greater in ventilated than nonventilated patients. Other risk factors include patients advanced age and personal habits (cigarette smoking and consumption of alcohol), underlying disease and co-morbidities, duration of ventilation, supine position, and improper use of antimicrobial therapy contributing to increased incidence of multidrug resistant (MDR) pathogens.6, 7
Economic complexities of HAIs are enormous and, unfortunately, often neglected. The burden of HAI represents a big challenge throughout the world.8 This challenge is more evident in developing countries, where infection prevention and control policies are either nonexistent, poorly adopted, or insufficiently funded.9
Kosovo has one of the highest prevalence rates of HAIs in Europe.10 A point prevalence survey performed in 2003 and 2006 in the University Clinical Centre of Kosovo (UCCK) showed an overall HAI prevalence rate at 17.4%; whereas a surveillance of ICU showed the prevalence rate of HAIs at 68.7%. Among HAIs, VAP was a predominant type of infection with a prevalence rate of 72.7%. 11, 12 The main reasons are believed to be lack of support for implementation of infection prevention policies (understaffed in ICU, reuse of single use devices, and very low compliance with hand-hygiene practices). Similar patterns have been confirmed by a systematic review covering some low- and middle-income countries, whereby VAP is emphasized as the most frequent type of HAI in some of the countries.13
The impact and the financial burden of VAP on the healthcare system and patients is enormous. This burden is even more emphasized in Kosovo considering over 40% unemployment rate, lack of health insurance system, lowest government healthcare expenditure in Europe, and the citizens’ out-of-pocket money almost matching the government public health spending.14
Assessing and understanding this financial burden would inevitably help to understand the actual situation as there is scarcity of data in Kosovo regarding the actual costs attributable to VAP or any HAI either from the provider or the patient perspective. Therefore, the aim of this study was to assess the financial burden of VAP, particularly in terms of the direct medical costs incurred by the patients treated in ICU of UCCK and examine potential prevention and control measures for Kosovo.
The study was approved by the Ethics Committee Board at the Ministry of Health. Since the protocol was observational, there was no need for patient consent. The UCCK serves as the only tertiary healthcare referral center in Kosovo for a population of around 1.8 million with 2,100 beds and over 60,000 admissions per year. It has one mixed ICU with 12 beds.
The surveillance was based on prospective observational studies, whereby (i) prospective cohort study had determined the incidence rates of HAIs, including VAP in ICU while (ii) (nested) casecontrol study had determined the affected patients, wherein matching was performed according to original reason for admission (e.g. traffic accidents, stroke, cancer) as well as mechanical ventilation (MV).
The surveillance was performed according to the International Nosocomial Infection Control Consortium (INICC) Outcome and Process Surveillance guideline.15 Criteria for defining VAP were those recommended by Centers for Disease Control (CDC).16 The decision of VAP or colonization was made according to the laboratory and clinical findings. The data were collected by ICU staff directly from the ICU patients’ medical charts using INICC standard questionnaires and were further imported by NIPHK staff into their database where it was fully protected. The NIPHK mainly focused on clinical microbiology, laboratory and epidemiological data (pooled means with standard deviation and incidence density of VAP per 1000 ventilator-days) and did not perform any cost analysis. Multiple HAIs were excluded from the study as we aimed to detect costs only for VAP.
The study used the random surveillance dataset obtained during the 3-month period (April–June 2013). The dataset included all patients (66) in ICU, who were admitted and discharged during the surveillance period. The dataset included: age, gender, LOS in ICU, MV days, underlying disease or conditions, treatment therapy, and clinical outcome. Hematological and biochemical tests (daily), chest radiographs (2–4 times a week), and microbiological cultures from blood, nasopharynx, tracheal aspirate, urine, and wounds (on admission and twice a week) were performed routinely.
Unfortunately, due to budgetary limitations, a considerable number of drugs and supplies necessary for treatment of ICU patients are unavailable in the UCCK and have to be purchased by the patients’ families separately. Therefore, additional consultations were performed with ICU and NIPHK staff in order to establish accurate type and the number of drugs and supplies that had to be purchased for each of the patients during their stay in the ICU. As a result, the ICU patient medical costs included: (i) antibiotics, (ii) other treatment drugs, (iii) parenteral and enteral nutrition, (iv) medical supplies, and (v) laboratory tests (some of the laboratory tests had to be performed outside UCCK in private laboratories). Patients’ nonmedical costs, such as transport and indirect cost (patient time and cost and time of family members visiting the patient regularly) or costs incurred by the provider are not included in this analysis. Additional costs, such as unofficial payments to medical staff might have occurred to patients or their families. However, this has not been a subject of this study, and therefore, has not been studied.
The main focus of this analysis was to compare the cost differences between VAP and non-VAP patients. Statistical analyses were performed using MedCalc statistical software version 16.2. P value <0.01 was considered as statistically significant. Cost analysis included means (with standard deviation), medians (with 25–75% inter-quartile range), and statistical tests (t test) for different cost information, such as (i) total direct medical costs, (ii) antibiotic costs, (iii) other medicines costs, (iv) medical supplies costs, and (v) laboratory costs.
A health economic evaluation can be conducted from one or more perspectives, such as societal perspective, public-health perspective, healthcare system perspective, healthcare payer’s perspective, institutional perspective, and patient’s perspective. Costs from the patients’ perspective are the expenses that patients pay for medical products or healthcare services not covered by their health insurance. For health outcome studies using the patient’s perspective, outcomes are commonly examined in terms of health-related quality of life, patient preference, and the portion of healthcare costs that the patients are responsible for. The prices were determined based on an average of three pharmacies and laboratories located in the vicinity of UCCK, where most of the drugs and supplies were purchased and laboratory analysis were performed. Calculations of direct medical costs were performed for every patient individually, and then compiled into Microsoft excel for further analysis. Both the surveillance and costs data were stored and analyzed in Microsoft excel file format.
The underlining purpose of this approach was to determine the financial burden VAP had on total patient medical costs. As the information regarding patient’s income could not be accessed the analysis could not measure the real burden on their income due to VAP. For easier comparison all references to cost are in Euro currency.
During the surveillance period, (April–June 2013) all patients (66) who were admitted to ICU/UCCK were included in the study as they underwent MV and stayed for ≥48 hours. Of these 66, the gender breakdown is relatively balanced with 28 (42.4%) female and 38 (57.6%) male patients. The age ranged between 1 and 83 years with a mean age of 34.30±23.81 years. The ICU surveillance results showed an overall incidence rate of HAIs a s 62.12% with VAP being the most frequent type of infection at 73.17%.
Almost half of the ICU patients developed VAP (45.45 %) with VAP incidence density standing at 57.47 per 1,000 ventilator-days. Mean total direct patient costs in the VAP group were significantly higher compared to those in the non-VAP group (€647.12±487.67 vs. €227.22±174.13). Equally, the median total direct patient costs are higher in the VAP group compared to the non-VAP group (€464.70± 164.18). This phenomenon is consistent throughout other cost components, which confirms that the differences between VAP and non-VAP patients are statistically significant (Table 1).

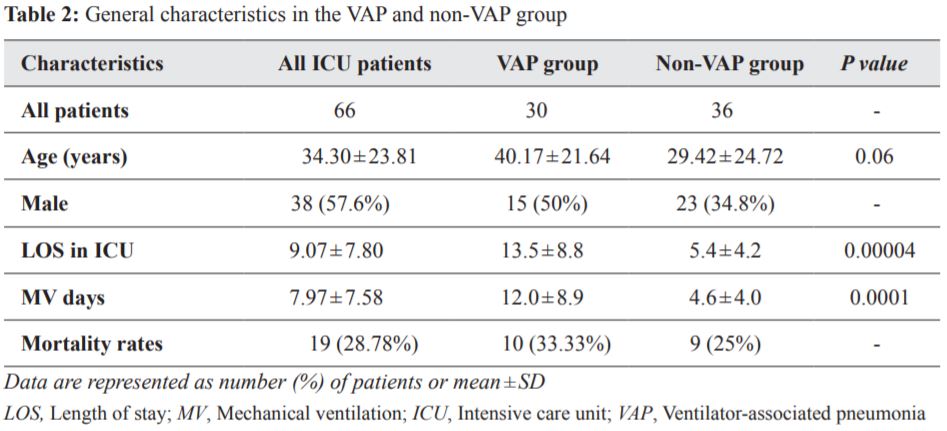
Similar pattern is observed in other general characteristics which were all higher in the VAP compared to non-VAP group of patients as follows (Table 2):
(i) LOS in the ICU was 13.5±8.8 days in the VAP group compared to 5.4±4.2 days in the non-VAP group (P<0.001).
(ii) MV was 12.0±8.8 days in the VAP group compared to 4.5±3.9 days in the non-VAP group (P=0.0001).
(iii) Mortality rates were also higher in the VAP group (33.33%) compared to non-VAP group (25%).
Studies related to costs attributable to VAP recognize the fact that there is a great discrepancy between findings due to differences in the costs analyzed, charges, or study objectives. This could limit the relevance of comparison between studies in terms of understanding the real financial burden of VAP.17, 18 Another limitation could be related to the issues of diagnosis of VAP, which brings into question the real number of affected patients, their LOS, and costs attributable to VAP.19
For years, the issue of HAIs in UCCK has been neglected and its real rates have not been openly presented to the public, to the contrary they were often denied.20 Increased rates of HAIs in the UCCK, and its ICU in particular, are linked to budgetary limitations, old and under maintained facilities, low staff compliance on infection control and prevention practices, outdated equipment, and uncontrolled use of antibiotics, which subsequently contributed to higher rate of antimicrobial resistance.
Comparison of direct medical patient cost in the ICU of UCCK with studies of the other countries has proven to be rather difficult. All studies report VAP costs from the hospital perspective as there is an established health insurance system, wherein VAP patients have insurance and don’t have to pay randomly. In addition, other countries have different socioeconomic situation, services, medicines, and medical charges than that of Kosovo. In Kosovo, patients are often required to purchase most of antibiotics and therapeutic drugs, parenteral and enteral nutrition, some specific medical supplies, and cover some of the laboratory tests that are not performed in the UCCK.
Considering Kosovo’s socioeconomic situation, the results of VAP cost analysis are staggering as the mean total patient cost for an episode of VAP is in the range of €647 for an average ICU LOS of 13.5 days. In actual terms, this cost represents around two average monthly salaries in Kosovo. A recent WB report claims that an estimated per capita gross domestic product (GDP) in Kosovo is around €2,600, which makes it one of the poorest countries in Europe.21
The total ICU costs of patients are believed to be even higher considering that indirect cost of lost earnings, cost of family member’s time, and additional costs of further treatment after ICU discharge are not included in this analysis. Furthermore, it is estimated that the societal costs of VAP in Kosovo are much higher, considering that providers charge in terms of additional staff time, equipment depreciation, cost of drugs and medical supplies, and radiology and microbiology services, which have not been accounted for. For example, the NIPHK has confirmed that it had to microbiologically examine 243 different samples obtained from the ICU patients during the surveillance period. This makes the notion of societal and opportunity cost of VAP occurrence even more debatable. Considering the above facts and the findings of this report it is evident that VAP represents a huge financial burden for both Kosovo healthcare sector and its citizens.
Cost studies in the literature show that other countries have their own challenges with VAP. Studies from Switzerland22 and Germany23 seemingly show more complete picture of VAP cost as the costing is based on common parameters, such as ICU stay and direct medical (staff time, therapy, medical supplies, and diagnostics) and non-medical (administration and maintenance) costs. Issues related to case definition and diagnostic procedures of VAP represent an additional challenge in terms of the real VAP cost and its cost control. There are certainly other parameters, such as litigation, which might affect and increase the actual VAP cost to hospitals, however, are not sufficiently described or considered.24
In a systematic review by Arabi et al. on VAP in adults in limited-resource countries from 1966 to 2007, the rates of VAP were higher than the CDC’s NHSN benchmark rates and ranged from 10 to 41.7 per 1000 ventilator-days. The review found that the crude mortality attributable to VAP ranged from 16–94%.25 To calculate the cost of HAI in ICUs, a 5-year matched cohort study undertaken at six ICUs in Argentina showed that the mean extra antibiotic cost was $996, the mean extra total cost was $2,255, and the extra mortality was 30.3%.26
Cost attributable to VAP is estimated to be around €4,700 in Turkey27 compared to €13,144 in Switzerland22 and €17,015 in Germany23. Amongst others, these differences probably exist due to country specific economic situation, which could be well documented through country specific GDP per capita i.e. €7,900, €30,750, and €58,557 in Turkey, Germany, and Switzerland, respectively.28 To counter these cost differences, it is assumed that LOS in the ICU is a more accurate proximation for estimating and understanding the real burden of VAP.29 Further, this can certainly be confirmed in the case of the reviewed studies and Kosovo findings, wherein LOS attributable to VAP ranges between 8 and 10 days.
One of the limitations of our surveillance dataset could be that it did not contain information about previous infection patterns, antibiotic use, or hospital stay prior to ICU admission. This could have had confounding effects on results. Another confounding factor could have been the fact that antibiotic therapy was administered to all patients, in some cases even from day one and before getting clinical and microbiological confirmation of VAP. This pattern of routine antibiotic use could have affected the patients’ costs.
As a recommendation from this study, Kosovo’s Ministry of Health should implement Health Insurance Law at the earliest. This law foresees universal coverage, whereby every Kosovo citizen will need to be insured by self-purchased premium and also participate with some co-payments. The UCCK should improve its organizational and management capacities in terms of ICU-related VAP prevention and control measures.
In conclusion, despite big cost discrepancies and difficulty in comparing the data, our study implicates that development of VAP leads to additional cost and prolonged ICU LOS. Further, our study can provide evidence for decision-makers and healthcare providers on the need to apply stringent rules on VAP prevention and control programs in Kosovo.
The authors of the study declare no conflicts of interest.
Samir Selimi is thankful to Ms. Jo Borghi, Supervisor at London School of Hygiene and Tropical Medicine, for her advice, guidance, and unreserved support during the entire period of project report development.