
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 1, Pages 8-13
https://doi.org/10.26715/jbms.p25_3Shereen Hussain1*, Reham A. Al Garf2
1Primary Care, Ministry of Health, Kingdom of Bahrain, Senior Lecturer, RCSI, Kingdom of Bahrain
2Primary Care, Ministry of Health, Kingdom of Bahrain
*Corresponding author:
Shereen Hussain, Primary Care, Ministry of Health, Kingdom of Bahrain, Senior Lecturer, RCSI, Kingdom of Bahrain, Email: SHejji@health.gov.bh

Background: Depression is the second most common chronic disorder seen by physicians in primary care, where an average of 12% of patients might present with major depression. Depressed patients are more likely to see a primary care physician than a specialist for both initial diagnosis and treatment.
Methods: As part of the celebration for the Gulf Youth Day in October 2012, fifty-five students were invited to Naim Health Centre. The patient health questionnaire was distributed to them to screen for mental disorders. The students were given instructions on how to complete the questionnaire and the participating clinicians scored the responses and summarized the results.
Results: Nine students had major depressive disorders and fifteen students had other depressive disorders. Seven of the students with major depressive illness had suicidal ideation compared to nine out of the fifteen students with other depressive illnesses. In addition, seven of the students who tested negatively for depressive illness, still had suicidal ideation.
Conclusion: It is critically important that primary care practitioners are able to correctly identify patients suffering from depression. Screening is a very effective first step in the detection, diagnosis, and treatment of depression in primary care. However, the skillful clinical interview which incorporates verbal communication and good interpretation of non-verbal clues is crucial and indispensable for effective and reliable diagnosis.
Keywords: Depression, Adolescents, Primary care, Screening, Self-reporting questionnaire
The second most common chronic disorder seen by primary care physicians is depression,1 with an average of 12% of patients presenting with major depression.2 The degree of suffering and disability due to depression is comparable to that occurring with most chronic medical conditions.3 Early detection and appropriate treatment can have significant positive impact in most patients with depression.4 The majority of patients with depression can be effectively treated with pharmacotherapeutic and psychotherapeutic modalities.5 Depression has no age boundaries, and may occur during any period of life: childhood, adolescence, adulthood and old age. It can present as a combination of negative feelings and somatic symptoms such as fatigue, sleep problems, pain, loss of interest in sexual activity, or multiple, persistent vague symptoms.6 In general, depressed patients are more likely to see a primary care physician than a specialist for both the initial diagnosis and subsequent treatment. In a primary care setting, it can be quite challenging to recognize depression especially when it comes to men who usually have difficulty exploring their emotions. Equally important to note is that depressed patients who present at the primary care level often describe somatic symptoms.7
Longitudinal data from the World Health Organization Psychological Problems in General Health Care study were used to examine the relationship between recognition and outcomes among depressed primary care patients. A representative sample of primary care patients at 15 sites completed a baseline assessment including the Composite International Diagnostic Interview (CIDI), the 28-item General Health Questionnaire (GHQ), and the Brief Disability Questionnaire (BDQ). The GHQ and BDQ were re-administered after 3 months, and the GHQ, BDQ, and CIDI were re-administered after 12 months. In the study, almost half (42%) of the 948 patients with major depression were identified by the primary care physician and so were given an appropriate diagnosis.8 Depression cases that were either under-detected or undertreated led not only to unnecessary suffering, functional impairment and higher risk of suicidal attempts, but also to a loss of occupational productivity, and inappropriate use of general medical services.9
Mental and psychological problems are reported to occur in around 450 million of the world’s population, yet the majority will be either incorrectly diagnosed or undertreated.10 Treating depression can be very challenging, because to secure improvement in outcomes requires not only prescribing new treatment but also organizational and functional changes in healthcare teams in line with those given to other chronic disease.11 A number of randomized controlled trials have shown that enhanced care of major depression can lead to a better outcome than patients with depression may usually receive.12 Moreover, although enhanced care may moderately increase the cost of treatment per patient, ultimately it remains more cost effective than standard care.13,14
Care of depression in primary care Specialist support has been shown to improve patients’ outcomes. Success was reported in trials which examined taking responsibility for patient compliance, and assessing whether depressive symptoms were improving and whether treatment guidelines were followed, or if other unexpected, important factors emerged. Significantly, in many of these trials these services were provided over the phone and at low cost per case treated.
Effective interventions usually incorporated new and economical approaches to the integration of specialist support into the primary care of patients presenting with depression. In some interventions these included a psychiatrist’s supervision of the case manager to provide input on difficult clinical situations, to provide advice and support for the treating physician or to take over when patients with more difficult problems needed an effective plan for treatment. A focus on low-cost management of cases, along with flexible and accessible working relationships between primary care physicians, case managers and mental health specialists, is the best way forward and is supported by high level evidence. This makes it possible for most patients presenting with depression to be able to access effective treatment at the primary care level, while the remainder that need ongoing care are identified and referred to specialists.9
There are a number of related factors that could contribute to low detection rates, such as patients presenting with unexplained somatic symptoms rather than directly presenting with symptoms of depression and physicians not having sufficient time to ask the appropriate questions during the clinical consultations.15 However, several factors might contribute to an improved detection of depression in these patients and must be taken into consideration.16 These include a previous history of depression, family history of depression, substance dependence (to a lesser degree, substance abuse), female gender, other mental disorders, cognitive and behavioral factors often witnessed in depression, as well as chronic stressors and childhood trauma, particularly physical and/or sexual abuse.17 A number of screening instruments also incorporate multiple modules which can be useful in alerting the physician to other medical or psychological conditions such as substance abuse, eating disorders and anxiety.
The US Preventive Services Task Force (USPSTF) in 2009 reviewed studies of screening for depression in children and adolescents in primary care settings. Although they did find some evidence suggesting that screening could detect depression in adolescents, they came to the conclusion that overall there was insufficient evidence to recommend or disapprove of the routine screening of children and adolescents at the present time.18 The USPSTF concluded that screening did increase the rate of detection of depression by an average factor of 2 to 3, with an absolute increase in diagnosis ranging from 1 to 47 points. However, they emphasized that the results of the screening alone were not sufficient to rule out other potential causes of patients’ symptoms and would not permit an absolute diagnosis of depression.17 In contrast, in its Guidelines for Adolescent Preventive Services, the American Medical Association recommends that adolescents should be screened for depression if the following cumulative risks are visible: deteriorating school grades, familial dysfunction, homosexual orientation, alcohol or other drug use, chronic melancholy, a history of suicidal attempts and suicidal plans.19
A number of assessment tools that can detect depression are available, including various self-administered scales.20 Yet these scales might be less specific for major depression and other mood disorders and might have a low rate of accuracy in discriminating depression from anxiety or even general psychological distress. Detecting depression and beginning treatment are crucial, yet often insufficient, steps to improve outcomes at the primary care level.21 The monitoring of clinical response to therapy is also critical. Various studies have demonstrated that monitoring is often inadequate, resulting in the failure of clinicians to detect noncompliance with treatment and medication, failure in increasing the dosage when needed or failure in prescribing psychotherapy when required.22
As part of the celebration for the Gulf Youth Day in October 2012, fifty-five students were invited to the Naim Health Center. During this event, the students’ blood pressure, weight and height were measured; they attended a lecture about the period of adolescence which was presented to them by a social worker and an exhibition about the adverse effects of smoking. The Health Center team members involved in that activity consisted of doctors, public health nurses, a social worker and a health educator. The patient health questionnaire (PHQ) was distributed to the students to screen for mental disorders. They were given instructions on how to complete the questionnaire and were not obliged to write their names and hence they were assured that their answers would remain anonymous and confidential. The PHQ-9 Depression Screener is accessible at http://www.phqscreeners.com and is available in a variety of languages, including Arabic. The Patient Health Questionnaire (PHQ) was developed to smooth and simplify the recognition and diagnosis of the most prevalent mental disorders in primary care patients. The PHQ Depression Severity Index score can be calculated and used to monitor change over time in patients with depressive disorders. This is calculated by assigning scores of 0, 1, 2, and 3, to the response categories of “not at all,” “several days,” “more than half the days,” and “nearly every day,” respectively. The total score for the nine items included in the PHQ-9 can range from 0 to 27. Cut-off points for mild, moderate, moderately severe and severe depression are scores of 5, 10, 15, and 20, respectively.23 While students were busy with other activities, the clinicians and other team members were scoring students’ responses and summarizing the results. At the end of the day the students were invited to attend an open meeting with the clinicians. The objectives of the meeting were to explain the purpose and interpretation of the questionnaire and the future actions that should be taken by students to get help if needed. These discussions between participants and clinicians were very rich, open and interactive. The meeting was essential because the students were medically registered at another health center where they could receive treatments if required. At the end of the meeting contact numbers were given to students to facilitate discussions and to provide support if required.
The patient questionnaire The patient health questionnaire (PHQ) is a three-page, self-administered version of the primary care evaluation of mental disorders (PRIME-MD) that has been well validated by two major psychology clinics. The PHQ is now the most commonly used version in both clinical and research settings. With nine questions, the PHQ-9 is half the length of some of the other depression measures, has comparable sensitivity and specificity and consists of the actual nine criteria on which the diagnosis of DSM-IV depressive disorder is based. The PHQ-9 is a dual-purpose instrument whose nine items can establish provisional depressive disorder diagnoses as well as the grade of depressive symptom severity [http://impact-uw.org/tools/phq9.html].
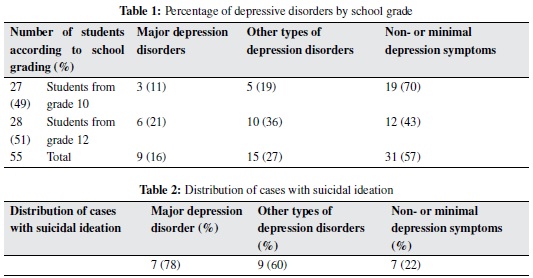
The total number of students that attended the activity and completed the PHQ-9 was 55: 27 from grade 10 and 28 from grade 12. Nine (16% of respondents) had a major depressive disorder, three from grade 10 and six from grade 12. Fifteen (27% of respondents) had other depressive disorders, five students from grade 10 and ten from grade 12. (See Table 1.)
Over three-quarters of the students (7) of those with major depressive illness had suicidal ideation compared to nine (60%) of those with other depressive illnesses. The study also found that seven (22%) of the students who tested negatively for depressive illness still had suicidal ideation. (See Table 2.)
The PHQ-9 was used instead of other depression scales for a number of reasons: availability of an Arabic version; it is shorter than many other depression rating scales; it can be administered in person, over the telephone or as a self-report; it facilitates the diagnosis of major and minor depression, it assesses depression symptom severity; it can be used to follow up response to treatment; and it is reliable in a variety of patients, including adolescents.
The number of students in this study was very limited, as it was conducted as part of a general activity. Despite the low number of participants, the results were similar to those of other studies. Nevertheless, the somewhat disturbing figures indicate the necessity for a larger and more formal screening study. These screening tests raise red flags to alert the physician to the possibility of depressive illness, which should then be verified by clinical interviews and further follow-up visits. One important observation of this study was the frequent discussion among students about psychological issues.
Major depressive disorders accounted for 16% and other depressive disorders 27% in our sample. This does not signify that these students suffered from depression, but clinical assessments should be done and other causes of these symptoms should be ruled out. The results show that the percentage of students with major depression was higher in those in Grade 12 compared to Grade 10, which is most likely related to academic factors, since an overemphasis on academic achievement which may, in turn, lead to stress and mental health problems.
The relationship between mental illness and suicide, self harm, is well-known. It has been estimated that mental disorder is associated with an 11-fold risk of suicide.24 Thirty-five percent of suicide cases with mental problem had depression. Suicide is the most common cause of death after road traffic accidents among male adolescents. Some 50% of adolescents who have previously attempted subsequently re-attempted.25 It is not surprising, therefore, that depressive illness is the most common single antecedent to suicide, and suicide is the commonest cause of death in effective disorders.
The rate of suicide differs from country to country, and countries such as Hungary, Japan, Finland, the countries of the former Soviet Union and Sri Lanka have the highest rate while some other countries, such as those in South America, southern Europe and some Islamic countries, have the lowest rate.26 This can possibly be explained by factors such as alcohol abuse, cultural and religious differences in help-seeking behavior, social attitudes to suicide, socioeconomic upheaval, and the availability of highly lethal methods of suicide.
Questioning the students during discussion about suicidal ideation revealed no significant suicidal potential in these groups, but we provided them with a contact telephone number in case they wanted to discuss the results of the questionnaire.
The fact that 16 students (67%) out of the positive cases of major and other types of depression had suicidal ideation is also a red flag that indicates that these students may need psychological or psychiatric support. Surprisingly, seven students who were negative for depressive disorder had suicidal ideation. The instructions accompanying the questionnaire recommend that suicidal ideation be documented and ‘counted’ whenever it is present.
How can we account for this unexpected finding? It could have to do with the social desirability bias, which is a well-documented concern with self-reporting methodology. Participants are usually unwilling, or might be uncomfortable, to share information that might misrepresent them within the context of their social environment, even if they are aware that their responses are entirely anonymous.
Therefore, it is possible to attribute this contradictory information to the sample age group, being teenagers, which leads to higher tendency to social desirability. Moreover, the sample’s social and religious norms may play another role, as suicide is forbidden in Islam as evidenced by the Hussain et al., following:
From the Quran:
“And do not kill yourselves; surely God is most Merciful to you.”
-The Holy Qur’an, Sura 4 (An-Nisa), Aya 29 (4:29)
“And do not throw yourselves in destruction.”
-The Holy Qur’an, Sura 2 (Al-Baqarah), Aya 195 (2:195)
From the Hadith:
“As narrated by Abu Huraira the Prophet said,Whoever purposely throws himself from a mountain and kills himself, will be in the (Hell) Fire falling down into it and abiding therein perpetually forever; and whoever drinks poison and kills himself with it, he will be carrying his poison in his hand and drinking it in the (Hell) Fire wherein he will abide eternally forever; and whoever kills himself with an iron weapon, will be carrying that weapon in his hand and stabbing his abdomen with it in the (Hell) Fire wherein he will abide eternally forever.” Sahih al-Bukhari, Volume 7, Book 71, Number 670 When we analyze the idea of adolescents’ heightened social desirability and the clear prohibition of suicide in Islam, how do we account for the number of survey participants who indicated suicidal thoughts, yet ultimately showed negative results in the survey? A possible explanation could be the other side of the coin when it comes to the teenage years: rebellion and the urge to push against the boundaries of social conformity. Their indication of suicidal thoughts, when we keep the concept of social desirability in mind, could be an indication of a form of rebellion against social and religious beliefs. Clearly, this is all theoretical speculation and more studies need to be conducted; however, it does make the argument that when considering social desirability, we must keep in mind the characteristics of our sample, including age characteristics and the prevailing social beliefs and norms.
More generally, our findings also alert us to the fact that we may need to include adolescents among those to be seen at mental health clinics as the latter only allow patients over eighteen years ofage, and thereby providing them with psychological support and diagnosing cases of depression in itsearly stages.
Although screening instruments help physicians identify their depressed patients more readily, to diagnose them more efficiently, and to increase the probability that these often-overlooked patients will receive treatment, they should not be used merely to diagnose patients. Physicians should not only account for screening test results cut-off points without confirmatory information, the results should be used as red flags to alert the physician to the possibility of depression. After that, more verification is recommended such as: clinical interview, chart review, physical exam, and, if necessary, lab work and further follow-up visits. Clinical assessments should be done and other causes of these symptoms should be ruled out during the course of the physician-patient interview. Questioning about the suicidal ideation must be clear and direct. Areas of patients’ strengths, impairment, relationships and support systems should also be evaluated during a personal interview. Screening instruments are important objective tools in measuring depression. However, in the event of negative screening results, the physician should not neglect key symptoms and risk factors of depression. These instruments also assess the severity and degree of depression based on the following factors; numbers of symptoms, duration of episodes, frequency of occurrence and the degree of functional impairment. Moreover, the instruments vary in terms of type and extent of information collected. Some collect information on the number of days patients experience symptoms, or the degree of functional impairment, while others collect information on the number of symptoms experienced over a certain period of time. In targeted adult patients, and other populations at high risk for depression, longer screening measures for depression are more appropriate than the shorter measures that are used in adult population screening.9,21,22
The period of adolescence is a crucial period in a person’s life as it is a time of transition from childhood into adulthood. During this period, adolescents have to face numerous challenges as they try to cope with multiple changes in their lives. It is vital to diagnose depression early in children and adolescents because if left undiagnosed and untreated it may persist into adult depression and increase the risk of nicotine dependence and alcohol dependence and abuse.
Depressed patients should be more readily identified by primary care practitioners. Some depression screening measures can help these physicians more effectively recognize and diagnose depression in their patients during the busy hours of their daily clinic. In primary care, screening is very valuable as a first step to treat and diagnose patients with depression.
It is extremely important to be aware of the potential biases of such instruments and how to overcome them. An essential concept which we have to keep in mind is that we are dealing with humans and although we may use instruments to help us identify patients’ problems they can never replace a skillful clinical interview which incorporates empathetic verbal communication and good interpretation of non-verbal clues for patient assessment.