
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 2, Pages 80-86
http://doi.org/10.26715/jbms.25_2_4Fatima Ahmed Al-Jurdabi,* Huda Al-Ebraheem**
*Consultant Family Physician, Head of Jidhafs Health Centre, Kingdom of Bahrain
**Consultant Family Physician, Naim Health Centre, Kingdom of Bahrain
Correspondence to: Fjirdabi@health.gov.bh

Background: Asthma is a serious public health problem, affecting people of all ages. When uncontrolled it can cause significant morbidity and mortality. Poor implementation of the guidelines is considered one of several barriers for achieving asthma control.
Objectives: To determine the asthma knowledge, attitude and prescribing behavior of primary health care physicians in the Kingdom of Bahrain.
Methods: A cross–sectional survey was carried out from March 2012 to March 2013 among primary health care physicians (PHC) attending asthma workshops as part of a continuing medical education program. During the study period 5 workshops were conducted which were attended by PHC physicians. A self-administered questionnaire was designed to achieve the research objective. The questionnaire was based primarily on a previous study carried out by the Chicago Asthma Surveillance Initiative (CASI) in the USA; a similar questionnaire was used in a study conducted in 2004, and permission was taken from the investigators to use it in our study. Questionnaires were distributed to the study groups at the beginning of each workshop and 192 of the 240 attending doctors completed the questionnaire, an 80% response rate.
Results: The responders were mainly family physicians (66.7%), of whom 73.4% were following asthma guidelines. The study showed that slightly more than half of PHC physicians (56.8%) were able to assess the level of asthma control appropriately and the majority of them reported scheduling regular follow-ups for their patients. However, only 39.1% of PHC physicians were aware of the appropriate medication recommended for step 1 and only 37.3% of them reported that they provided written plans for their patients.
Conclusion: Various aspects of GINA guidelines appear to have been integrated into clinical practice by primary care physicians in the Kingdom of Bahrain, whereas other recommandations do not seem to have been readily implemented.
Keywords: Primary health care physicians; bronchial asthma; PHC; Kingdom of Bahrain
Asthma is a common inflammatory disorder of the lungs, characterized by reversible airflow limitation and an increased airway hyper-responsiveness to a variety of stimuli, leading to recurring episodes of characteristic signs and symptoms.1
According to the World Health Organization (WHO), almost 300 million people suffer from asthma worldwide and with the rising trends it is expected to increase to 400 million by 2025. and nearly 255,000 people die annually from asthma.2 The prevalence is continuously increasing and is expected to rise by a further 100 million by the year 2025.3 A study in the United Kingdom showed an increase in the prevalence by more than 5.5-12%.4 In the Gulf and the region there is a paucity of data about the distribution of asthma, some studies have been carried out but they involved relatively small samples of patients. In Saudi Arabia the prevalence of asthma has been investigated in several studies and it has been found to have increased from 8% in 1986 to 23% in 1995.5-6
Increasing air pollution, rapid modernization, and widespread construction work are some of the reasons suggested for the increasing asthma problem, in addition to poor access to medical services, the high cost of effective drugs and poor health education among the affected population.7
Studies have shown that the majority of patients in developed and developing counties do not obtain optimal care, and therefore, are not well controlled.8 Poorly controlled asthma may cause significant morbidity and mortality whereas early treatment, proper administration of medication and monitoring of the disease can decrease the frequency of exacerbation, hospitalization and the mortality rate.9
In order to improve the quality of asthma care, several approaches have been attempted These include establishment of clinical guidelines for the diagnosis and management of asthma, such as GINA (Global Initiative for Asthma)10 and NAEPP (National Asthma Education and Prevention Program),11 as well as improvement of the knowledge and attitude of asthmatic patients and general practitioners by educational programs. Several guidelines have emphasized the perception of asthma as chronic inflammation of airways with stepwise use of anti–inflammatory medications.10-14 Despite this, previous studies suggest the existence of a gap between actual asthma care and guideline recommendations.15-18
The Ministry of Health in the Kingdom of Bahrain adopted the GINA guidelines in 2004 and some primary health care physicians have been trained to apply them in their practice. The authors are not aware of any previous local published studies on assessment of asthma management among GPs. Therefore, this study’s objective was to assess bronchial asthma knowledge, attitude, and the prescribing behavior of primary health care physicians in the Kingdom of Bahrain since the introduction of the guidelines.
A self-administered questionnaire was designed to achieve the research objective. The questionnaire was based primarily on a previous study carried out by the Chicago Asthma Surveillance Initiative (CASI) in the USA.19 A similar questionnaire was used by Abdulrahman Abudahish and Hassan Bella16 in their study which was conducted on 2004 and permission was taken from them to use it in our study. A slight modification of the questionnaire was made in order to comply with the new recommendations of GINA guidelines. The original questionnaire contained 7 case scenarios which were used in this study with minimal modification. We examined the assessment of level of asthma control instead of assessment of asthma severity for the first three cases and step 1 treatment as an alternative for treatment of intermittent asthma in adults and children for cases number four and five. All cases had a single correct response.
The questionnaire (see Appendix) contained 25 questions, most of which were multiple choice, aiming at assessment of three important aspects from the participating physicians; the physicians’ knowledge, practice and attitude. It covered mainly the following items:
The survey was carried out during the period from March 2012 to March 2013 among primary care physicians attending asthma workshops as part of a continuing medical education program (CME). During the study period 5 workshops were conducted and about 250 physicians attended. Questionnaires were distributed to the study groups before the beginning of each workshop and 192 of the 240 attending doctors completed it, a response rate of 80%. Scoring of case scenarios on asthma was used to determine the physicians’ knowledge.
The questionnaire was pilot tested on primary care physicians working in one primary care health centre. No significant alterations were required to the questionnaire following the pilot study so that the same questionnaire was used in the actual study.
Responses were coded and data were entered and analyzed using SPSS software (version 20). The mean ± standard deviation was calculated for numerical variables. Percentage was calculated for categorical variables.
The survey was completed by 192 of the 240 PHC physicians, a response rate of 80%.
• General Characteristics of Physicians
The responders were mainly female (67.7%) and 74.5% were Bahraini. Most of the physicians were family physicians (66.7%) and aged >34 years (70.8%). About 66% of the responders had been in practice for 10 years or more.
• Clinical Monitoring
The physicians were questioned on aspects of asthma monitoring and assessment of level of control. Table 1 illustrates that slightly more than half of PHC physicians (56.8%) were able to assess the level of asthma control appropriately.
Table 1. Scoring achieved by PHC physicians for case scenarios of asthma patients
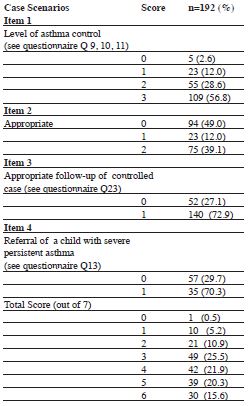
The physicians reported that during routine office visits, they most often monitored the following: day-time symptoms (92%), frequency of disturbed sleep (93.2%), activity level (91.7%), work/school days lost due to asthma (84.9%) and B2 agonist use (90%). Direct observation of inhaler techniques was reported by 72.4% of physicians and routine use of peak flow measurements was reported by 67.7%.
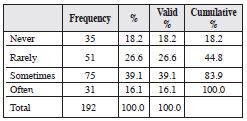
Physicians were also asked about their opinion regarding the usefulness of home peak flow monitoring for patients 5 years and over with moderate to severe persistent asthma. 51.6% of physicians described routine home peak flow monitoring as “often useful” and 41.1% reported it to be “somewhat useful.” Only 7.3% of physicians described home peak flow monitoring as not useful. However, 16.1 % of PHC physicians regularly checked peak expiratory flow during exacerbation (Table 2).
Table 2. How often do you use peak expiratory flow in acute symptomatic patients?
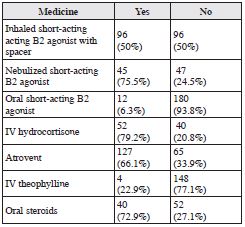
The survey also included questions on aspects of emergency care. As reported in Table 3, 75.5% of PHC physicians used inhaled salbutamol via nebulizer while half of them (50%) used the inhaled salbutamol via spacer. Additional treatment reported by PHC physicians during acute exacerbation of asthma included IV hydrocortisone (79.2%), oral steroid (72.9%) and atrovent (66.1%), whereas only 6.3% used oral salbutamol during exacerbation (Table 3).
Table 3. PHC physicians prescribing habits for patients with moderate to severe asthma attack
• Medication Used in Treating Patients With Asthma
The survey investigated physicians’ awareness of the medication recommended for step 1 for adults and children, and revealed that only 39.1% of them were aware of appropriate medicine (Table1).
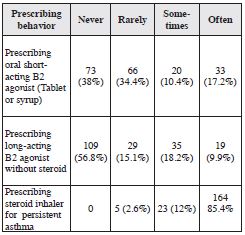
In their practice 72.4% of physicians never or rarely prescribed oral short-acting B2 agonists. However, 17.2% still prescribed oral short-acting B2 agonist very often and about 10.4% prescribed it sometimes. 71.9% of physicians reported that they had never or rarely prescribed longacting B2 agonist without inhaled steroid (Table 4). The majority of the respondents (85.4%) reported that they had prescribed inhaled steroids for persistent or uncontrolled asthma (Table 4).
Table 4. Prescribing behavior of PHC physicians on management of asthma
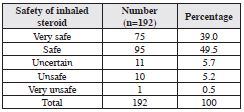
The survey also enquired about the participants’ opinions on the safety of inhaled corticosteroids at standard agreed doses. This we have reported in Table 5 which shows that 88.5% of the PHC physicians perceived inhaled corticosteroids as safe medicine, whereas only 5.7 % considered it as unsafe medicine.
• Other Aspects of Asthma Management
Awareness of the guidelines was high in that 73.4% of the physicians were following asthma guidelines. GINA guidelines were the most used (68.2%) and the majority (94.3%) of respondents believed that following asthma guidelines would improve their clinical practice.
Table 5. PHC Physicians’ opinion regarding safety of inhaled steroids
 When asked about their approach for the follow-up of patients with moderate, persistent asthma under control, the majority of physicians (72.9%) reported scheduling regular follow- up visits. However, 27.1% of the physicians reported seeing patients only when they were symptomatic.
When asked about their approach for the follow-up of patients with moderate, persistent asthma under control, the majority of physicians (72.9%) reported scheduling regular follow- up visits. However, 27.1% of the physicians reported seeing patients only when they were symptomatic.
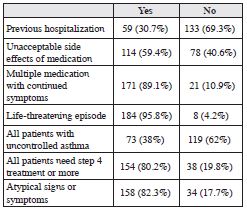
Referral to specialists was most often for patients with a history of life-threatening episodes (95.8%). Other reasons for referral include multiple medication with continuous symptoms (89.1%), the presence of atypical signs and symptoms (82.3%), uncontrolled patients on step four (80.2%) and the presence of unacceptable side effects of medication (59.4%). Less common reasons for referral included: history of previous hospitalization (30.7%) and all patients with uncontrolled asthma (38 %) as shown in Table 6.
Table 6. PHC physicians’ opinion about indications of referral for secondary care
The survey also evaluated the incorporation of patients’ health education into clinical practice. The majority of the physicians reported the following: discussion with the patient’s regarding mistaken beliefs (84.9%), the effect of smoking (95.8%), house dust mites (95.8%), animal allergens (93.8%) and the effect of cockroaches (67.2%).
When physicians were asked about the use of a written asthma action plans (WAAP) for their patients as a part of patient care, only 37.3% of them reported that they had used them.
The majority of respondents were aware of the availability of asthma guidelines; however, the survey did not ask whether the respondents have ever read the guidelines.
The results suggest that there are several key aspects in the delivery of asthma care by PHC physicians that are consistent with the guidelines’ recommendations. For example, the survey inquired into several aspects of peak flow use. Most of the responding physicians reported routine PEFR monitoring during routine office visits and half of them routinely use it for acute symptomatic patients. The study also tested the criteria for referral to specialists and it showed that most physicians would refer patients with life-threatening episodes and on multiple medications with continuous symptoms. Most of the PHC physicians reported scheduling regular follow-up for their patients which is consistent with the guidelines. However, the survey also identified several other aspects of asthma care that are less consistently observed in accordance with the guidelines’ recommendations. For example, the study showed that only 37% of physicians give their patients written instructions. The use of written asthma action plans is a key aspect of patient education, and their use has been associated with decreased morbidity.20 Tan et al. demonstrated in their study that GPs rarely used a written asthma action plan (WAAP) despite their perceived usefulness. This may be attributed to a lack of time related to patient loads in GP clinics and GPs lack of training and practice.21
In addition, the study showed that 28.1% of PHC physicians are still prescribing a long-acting B2 agonist without steroid. Its use as mono-therapy should be avoided as this may increase the risk of serious side effects in patients with unstable asthma.22 It has also been shown that 27.6% of PHC physicians prescribed an oral short-acting B2 agonist (SABA). Oral administration of SABA was not recommended because it has not been shown to be more effective than inhaled SABA and has been associated with an increased frequency of side effects.23
The study also disclosed that only about 44% of PHC physicians were unable to assess the level of control correctly and this may represent a major obstacle in managing asthma cases not only because of the lack of proper assessment but also because of inappropriate controller selection. Different studies have shown that continuous medical education can increase the knowledge of physicians after graduation especially in younger physicians.23 Unfortunately, our study did not investigate the proportion of PHC physicians who have ever participated in an asthma educational program.
Various aspects of the GINA guidelines appear to have been integrated into clinical practice by primary care physicians, whereas other recommandations do not appear to have been readily adopted. This information suggests areas for intervention such as improvement of physicians’ knowledge regarding proper assessment of the level of control and provision of appropriate management accordingly. This study also recommends further studies or audits to assess physicians’ adherence to the guidelines and to look for possible causes behind decreased compliance with the guidelines’ recommendations.