
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 2, Pages 87-92
http://doi.org/10.26715/jbms.25_2_5Fatima Habib*, Jameel Nasser*, Jaffer Abbas, Zahra AlMussali*, Nahla Madan*
*Consultant Family Physician, Ministry of Health, Kingdom of Bahrain
Correspondence to: zanrh64@yahoo.com

Objective: The aim of this study is to explore the beliefs and attitudes of primary care physicians (PCP) regarding insulin initiation in people with type 2 diabetes.
Methods: A structured, adapted questionnaire was distributed to all primary care physicians. The questionnaire consisted of 2 parts: the first part collected information on physicians’ demographic characteristics; the second part contained 30 items measuring the beliefs and attitudes of physicians regarding insulin initiation.
Results: A total of 171 physicians out of 245 completed the questionnaire with a response rate of 70%. Most of the physicians were between 30 and 59 years of age. The majority were females (79.4%), had been in practice for >10 years and were certified family physicians seeing more than 25 diabetic patients a week. About 75% of the physicians found initiation of insulin as one of the most difficult aspects of managing patients with type 2 diabetes. The main obstacles reported by physicians were: route of administration by injection, the risk of hypoglycemia, and the patients’ level of education. However, they agreed that the benefits of insulin outweighed the risks of hypoglycemia and weight gain. Only 45% of them agreed that patients will eventually need to go on insulin regardless of how well they adhere to treatment. Moreover, 31.8% of physicians stated that increased levels of plasma insulin will increase the risk of cardiovascular events.
Conclusion: Physicians’ concerns and lack of knowledge regarding insulin use may act as barriers to insulin initiation. This may increase the risk for a higher rate of uncontrolled diabetes and its subsequent complications.
Keywords: insulin; family physician; Bahrain
Diabetes is a common chronic non-communicable disease that is highly prevalent worldwide. It is estimated that the total number of affected people in 2013 was 382 million and it is expected that this number will rise to 592 million by 2035. Type 2 accounts for 85-95% of all diabetes1.
Hepatic and peripheral (muscle and fatty tissues) insulin resistance followed by β-cell dysfunction in susceptible individuals are the two major pathophysiologic defects that lead to type 2 diabetes2, 3. However, there are many other defects involving many different organs4, 5. Glycemic control is important to prevent and/or reduce the occurrence of micro- and macrovascular complications. It has been shown that reducing glycated hemoglobin (A1C) to ≤53 mmol/mol (7%) resulted in significant reduction of microvascular complications6. While intensive control has not been found to result in significant reduction of macrovascular complications (and can be hazardous to some patients) as shown in recent trials in newly diagnosed short and long term beneficial effect is evident7-11.
Type 2 diabetes is a progressive disease. It has been shown that with time, there is a need for more than one agent to control hyperglycemia. For example, maximum doses of sulphonylurea failed to maintain normal fasting blood sugar (< 6mmol/l) in 53% of patients within 6 years of treatment and required the addition of insulin4, 12, 13. In addition, it was found that while oral hypoglycemic agents (OHA) were preferred over insulin, most patients eventually need insulin14.
Disappointingly, a substantial proportion of patients are still above their target A1C despite the introduction of many new and costly medications15, 16. This has been attributed to many factors, including physicians’ inertia. Recent studies found significant delay in titration of OHA and/or initiation and titration of insulin in uncontrolled patients14, 17, 18.
Primary care physicians (PCP) play an important role in the management of diabetes. Studies have found that people with diabetes are mostly seen by family doctors and general practitioners19. Unfortunately, it has also been found that misconceptions, wrong beliefs, inadequate knowledge about insulin therapy are common among PCP20- 23.
The aim of this study is to explore the beliefs and attitudes of PCPs regarding insulin initiation in people with type 2 diabetes.
An updated list of primary care physicians working in the Ministry of Health was obtained from the Directorate of Primary Health Care in the ministry. The questionnaire was sent to all physicians through the head of council of each health center. The study was conducted during the period from August to October 2013.
In order to explore the beliefs of the PCP regarding insulin initiation in patients with type 2 diabetes, a structured questionnaire, adapted from a previous study,22 was used. Permission was given by the authors of that study to use the questionnaire. The original questionnaire consisted of 2 parts:
The first part collected information on physicians’ demographic characteristics which included: age, gender, years of experience, and specialty. In addition, these two questions were included: (1) The number of patients with type 2 diabetes seen by the physicians in a week; and (2) A question exploring the physicians’ knowledge regarding the glycemic goal for patients in three age categories.
The second part of the questionnaire contained 30 items measuring the beliefs of physicians. The physicians’ responses were assessed on a five-point Likert scale: strongly agree, agree, don’t know, disagree, and strongly disagree.
Data was analyzed using the Statistical Package for the Social Sciences (SPSS) software, versions 20. Frequencies were used to describe these categorical variables: age groups, gender, years of experience, specialty, number of patients seen per week, and treatment goal in different age groups. In addition, frequencies were calculated for the responses to the 30 belief items. One-way analysis of variance (ANOVA) was used to test the association between each of the belief-item responses and the physicians’ characteristics. P-value less than 0.05 was considered statistically significant. The study was approved by National Research Committee for Primary Health Care.
A total of 171 physicians out of 245 responded and completed the questionnaire with a response rate of 70%. One hundred and fifty (88.3%) of them were between 30 and 59 years of age. One hundred and thirty-one of them were females (79.4%) and one hundred and three (60%) had been in practice for >10 years. According to specialty, one hundred and twenty-five (73%) were certified family physicians. One hundred and twelve physicians (83%) were seeing more than 25 diabetic patients a week. Regarding glycemic control, one hundred and fifty (89%) agreed that HbA1c should be ≤53 mmol/mol (7%) for patients with type 2 diabetes younger than 50 years of age, one hundred and twenty-seven (76%) agreed with the same goal for those between 50 and 70 years of age, but only eighty-five (50%) agreed for those patients over 70 years of age.
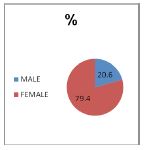
Figure 1. Gender distribution of physicians
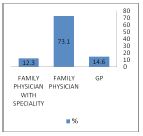
Figure 2. Physicians’ specialty
The responses to the research questions exploring beliefs about insulin initiation for type 2 diabetic patients were analyzed so that if 50% or more of responses fell into the ‘agree’ or ‘strongly agree’ category they were grouped together. Similarly, if <50% of responses fell into the ‘disagree to strongly disagree’ category, they were grouped together.
Table 1. Frequency distributions for items in which 50% or more primary care physicians (n=171) ‘agreed’ or ‘disagreed’ with the listed question*
*Available in pdf
Generally physicians agreed that the barriers to insulin therapy are route of administration being given by injection (items 1, 3, 6), and patients’ level of education (item 2). They also agreed that the benefits of insulin outweighed the risks of hypoglycemia (item 4) and weight gain (item 5). There is agreement that most of the patients on oral diabetes therapy are afraid of insulin therapy (item 8) and would be reluctant to accept a prescription for insulin (item 11). Many physicians (74.6%) also agreed that patients using insulin feel much better physically once they become accustomed to it (item 9), benefit from receiving insulin prior to the development of complications (item 10), and find the demands of insulin therapy to be less than they expected (item 12). About 75% of physicians found the initiation of insulin as one of the most difficult aspects of managing patients with type 2 diabetes (item 13). Many physicians (69.4%) agreed that most of their patients are using their insulin as prescribed (item 14). More than three quarters of physicians (76.3%) think that the risk of hypoglycemia from insulin therapy makes them reluctant to prescribe it for most of their patients ≥85 years of age (item 21). Regarding blood glucose monitoring, 49.7% of them find that their patients are self-monitoring their blood glucose with sufficient frequency (item 22). Only 52 % of physicians agreed that insulin therapy has a beneficial effect on insulin resistance (item 26). Some physicians (61.2%) disagreed that training in the proper administration of insulin is complicated for the patients (item 17). They also disagreed (78%) that the risk of weight gain associated with insulin therapy will make them reluctant to prescribe it for patients with BMI >35 (item 19) or that the fear of side effects is a barrier to the acceptance of insulin therapy (item 20).
The table below shows areas of disagreement between physicians.
Table 2. Frequency distributions for items in which <50% of primary care physicians ‘agreed’ or ‘disagreed’ with the listed question*
*Available in pdf
On bivariate analysis, there was a significant association between the gender of the physicians and the following items: (1) patients would initiate insulin therapy if it was not by injection (p=0.01), (3 ) the injection route of administration is the greatest barrier to acceptance of insulin (p=0.005), (6) physicians might prescribe insulin more frequently if the route did not involve injections (p=0.006), (12) patients find the demands of insulin therapy to be less than they expected (p=0.01), and (15) patients on oral therapy would regard the initiation of insulin as a personal failure (p=0.014). Moreover, there was a significant association between the specialty of the physicians and the following items: 3 (p=0.004), 13 (p=0.005), 18 (p=0.003), and 19 (p=0.004). On further analysis using one-way ANOVA procedure, a significant association between the years of experience of the physician and items 2 (p <0.001) and 13 (p=0.04) was shown. However, one-way ANOVA procedure did not show a significant association between the number of diabetic patients seen per week and any of the items.
There is a decline in ß-cell mass and function within 10-15 years after diagnosis of diabetes. Insulin is recommended if oral hypoglycemic agents failed to achieve good glycemic control in these patients12, 13, 24 .
A meta-analysis study concluded that “early and intensive antidiabetes treatment was recommended in patients with T2DM, particularly those with a shorter duration of disease and without a history of CVD” in order to prevent longterm complications of the disease 25.
Basically, most of these patients are managed by primary care physicians in the health centers. A Canadian study proved that PCPs could guide patients to implement bedtime basal insulin therapy as successfully as diabetes experts could and achieved glycemic control in their that PCPs should be given a practical protocol for initiating insulin26.
However, there are many factors delaying or preventing prompt insulin initiation. A study showed that insulin is underused in patients with type 2 diabetes despite the physicians’ knowledge of glycemic targets and this has been referred to as “clinical inertia”. The study found that PCPs added insulin late in the course of disease and waited an average of 9.2 years before initiating insulin. Furthermore, after more than 3 years of insulin therapy, 20% of patients still had poor glycemic control27.
So, in this study, barriers facing primary care physicians when prescribing insulin were explored. The response rate was satisfactory as 70% of the physicians responded and completed the questionnaire. Most of the physicians were between 30 and 59 years of age. The majority were females (79.4%), had been in practice for more than 10 years and were certified family physicians seeing more than 25 diabetic patients a week. Most of the physicians agreed that the goal for HbA1c should be ≤7% for patients with type 2 diabetes younger than 70 years of age, but only half of them agreed for those patients more than 70 years old. About 75% of physicians found the initiation of insulin as one of the most difficult aspects of managing patients with type 2 diabetes. There was a strong association of this belief with the physicians’ specialty and years of experience. The main obstacles reported by physicians in this study were: route of administration being given by injection, the risk of hypoglycemia, and patient’s level of education. The reporting of these obstacles was strongly associated with the physicians’ gender and specialty. These are shared factors and were reported by different similar studies22, 28. In another study physicians reported that they “have concerns about the use of insulin therapy in elderly patients and that “It is difficult to provide guidance and education on insulin injection to patients”28.
There is agreement among physicians that most of the patients on oral diabetes therapy are afraid of insulin therapy. This was also reported by other studies which found out that fear of difficulties with using insulin was the main obstacle facing these patients 22, 29.
On the other hand, physicians agreed that the benefits of insulin outweighed risks of hypoglycemia and weight gain. Many physicians (75%) also agreed that patients using insulin feel much better physically and benefit from receiving insulin prior to the development of complications (86%). These beneficial effects were reported by the patients themselves in a study which examined patients’ attitudes toward insulin injections and found that positive attitudes towards insulin are: “its efficacy and efficiency, the avoidance of complications, and feeling better and more energetic”30.
Although only 29% of physicians thought that training in administration of insulin is complicated for patients, 69% of them reported that patients take their insulin as prescribed. Several negative attitudes explained by patients for non-adherence were: anxiety about the pain, proper techniques, and hypoglycemic symptoms30. Another study showed that 94% of their patients adhered to their insulin regimen although they reported that the cost and weight gain were the main factors contributing to non-adherence. Moreover hypoglycemia was experienced by 56% of the participants. Some patients were uncomfortable with the use of insulin and others felt that taking insulin interfered with their routine activities31.
Physicians disagreed (78%) that the risk of weight gain associated with insulin or the fear of side effects will make them reluctant to prescribe it, but these side effects are of concern to many patients as reported by other studies21, 29, 31.
The results showed that PCPs may lack the knowledge about the progressive nature of diabetes mellitus as only 45% of them agreed that patients will eventually need to go on insulin regardless of how well they adhere to treatment. Moreover, 31.8% of physicians stated that increased levels of plasma insulin will increase the risk of cardiovascular events and 39.4% were neutral about that statement. These effects were not evident from previous research32.
Physicians’ concerns and lack of knowledge regarding insulin use may act as barriers to insulin initiation. This will delay achieving glycemic control and exposing patients to complications. Further studies are needed to look at factors that make patients reluctant to accept insulin therapy. Also factors related to health care system which facilitate the prescription of insulin should be explored. These include medical education of physicians, health education of patients and provision of medical supplies.
Author contribution: This is to certify that all authors have made a substantial contribution to:
(1) the concept and design; acquisition and analysis and interpretation of data;
(2) drafting the article and revising it critically for intellectual content and conformity to style guidelines; and
(3) final approval of the manuscript version to be published.
Potential conflicts of interest: none
Competing interest: none
Sponsorship: none
Ethical approval: Ministry of Health Research Committee.