
Journal of the Bahrain Medical Society
Year 2018, Volume 30, Issue 3, Pages 1-4
https://doi.org/10.26715/jbms.3_18112018Ahmed Al-Qattan1* , Sara Al-Saad2, Mohammed Almuharraqi1, Abdulla Darwish2, Khalifa Alghatam1
1Departments of Dental/Maxillofacial, BDF Hospital- Royal Medical Services, Kingdom of Bahrain
2Department of Pathology, BDF Hospital- Royal Medical Services, Kingdom of Bahrain
*Corresponding author:
Ahmed Al-Qattan, Departments of Dental/Maxillofacial, BDF Hospital- Royal Medical Services, Kingdom of Bahrain, Tel.: (+973) 66603636, Email: ahmedalqattan55@gmail.com
Received date: August 12, 2018; Accepted date: November 18, 2018; Published date: December 31,
2018

Central giant cell granuloma (CGCG) is an infrequent benign bony lesion of unpredictably aggressive behavior. The precise lesion character is debatable and remains inconclusive. However, three main theories were proposed: a sensitive lesion, a kind of neoplasm, or a developmental anomaly. This is a case presentation of a 16-year-old boy with a dental history of extraction of the lower right first molar, presented to hospital with two months history of swelling in the aforementioned area after the procedure. First biopsy of the swelling was performed outside the Kingdom of Bahrain. As per histopathological findings, the swelling was described as pyogenic granuloma. Second biopsy with necessary workup was conducted in the Kingdom of Bahrain and was confirmed as central giant cell granuloma through histopathological analysis; it was removed surgically.
Keywords: Central giant cell granuloma, histopathology, intraosseous, mandibular lesion, surgical excision
In 1953, Jaffe coined the term giant cell reparative granuloma (GCRG) to discriminate these lesions from giant cell tumor of long bones.1 He described it as a reactive jaw lesion occurring due to trauma, resulting in intraosseous hemorrhage containing giant cells. Later, the term GCRG was changed to central giant cell granuloma (CGCG).2, 3 CGCG is a benign, proliferative, intraosseous, and non-odontogenic lesion of unfamiliar etiology.4 Incidence of CGCG is estimated as 0.0001%, among which 60% cases aged < 30 years. Female to male ratio of the disease is 2:1.5, 6
Although, CGCG mostly occurs in the jaws and facial bones, it may also occur in other parts of the body. However, it is more often noticed in the mandible than in the maxilla. These lesions are detected usually in anterior region of the jaws and mandibular regions, many a time it crosses midline. It is moderately an uncommon pathological ailment accounting for < 7% of benign lesions in the jaws. Indistinguishable lesions may occur among the genetically disordered patients, such as those with Noonan syndrome, neurofibromatosis type I, or cherubism.2, 3, 5, 6
A 16-year-old boy reported to the Bahrain Defence Force Royal Medical Services maxillofacial outpatient department with two months old record of swelling above the right mandible area. The swelling started after the removal of severely putrefied lower right first molar. Trauma and/or family history of similar presentation was denied by the patient.
The patient sought medical treatment abroad and informed that a biopsy of the swelling revealed pyogenic granuloma. After a month of removing the abrasion at Sudan, asymptomatic inflammation reoccurred, gradually enlarging into facial disfigurement, which was evident during case presentation.
On visual and/or general examination, the boy was moderately built and well-nourished with no prior medical illness. A facial asymmetry due to a poorly-defined swelling was observed, measuring approximately 4 × 3 cm at the right angle of mandible, rendering the mandible boundary, which is difficult to palpate. The overlying skin seemed to be normal, while the enlargement itself was bony, hard, and non-tender to palpation (Figure 1). It was unraveled that the growth in size was fast, without any pain of mandible on the affected side.
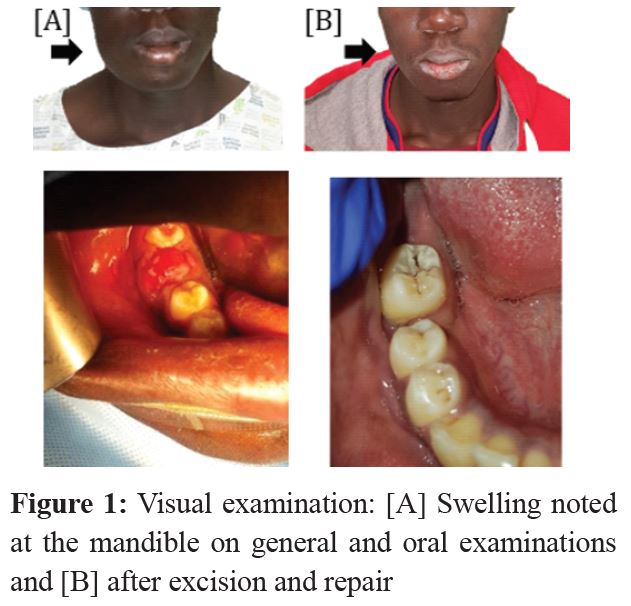
Medical observations revealed unevenly enlarged right mandibular body, hard consistency without redness, and right inferior alveolar nerve paresthesia. Intraoral examination revealed gingivobuccal sulcus elimination by exophytic growth in relation to 46 regions, which was hemorrhagic, soft, and slightly tender on palpation with the extension of the alveolar ridges.
Buccal vestibule diffuse swelling (2.5 × 2 cm) was observed in the same region and the tooth socket appeared infected, which might be the cause of inflammation. The intraoral enlargement was slightly tender and bony and hard on palpation with some areas of fluctuance in the buccal aspect. The adjacent dentition and the oral mucosa were normal (Figure 1).
The patient underwent in cone beam computed tomography (CBCT) with dental reformatting procedure (on demand 3D). It revealed a hypodense, distinct multilocular radiolucent, nonmineralized osteolytic lesions with some hyperdense hemorrhagic regions within the lesion. These lesions were positioned in the right mandibular angle and ramus with proximal-mesial extension (3 × 4 cm) and spreading, comprising the right mandible body with distinct and sclerotic boundaries excluding in the region of the superior aspect (Figure 2). The differential diagnoses were amelobastoma, CGCG, and tubercular osteomyelitis.
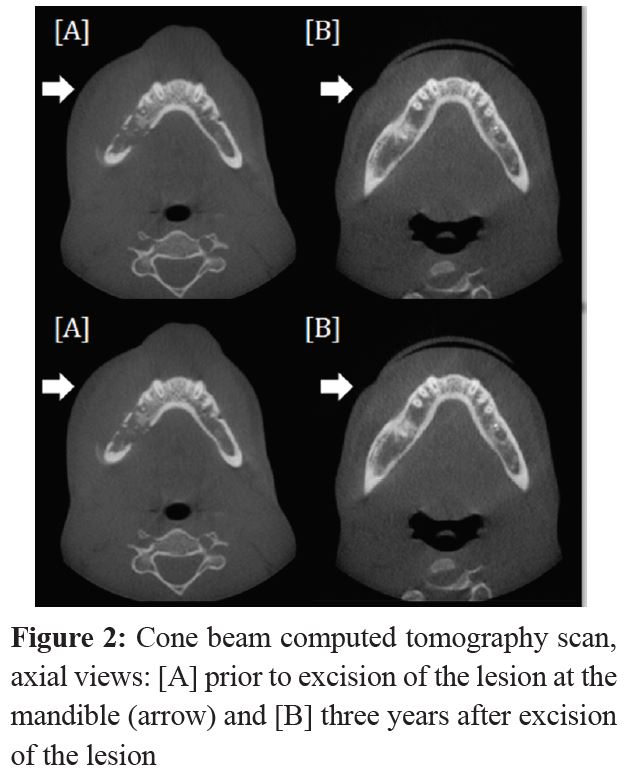
The CBCT lesion imaging showed the thinned lesion, with cortical bone margins extended and interrupted on lingual and buccal sides of the mandible, involving the right mental foramen, the right mandibular canal, several teeth roots and soft tissues adjacent to them.
The surgical procedures were performed under general anesthesia and the lesion was enucleated en masse followed by debridement. Smoothing out of the internal defected wall was done using a round bur. The defect was then filled with a spongy bone substitute and the defect orifice was sutured shut with a vicryl 3-0 interrupted and continue technique. The histopathological diagnosis was performed on the excised lesion.
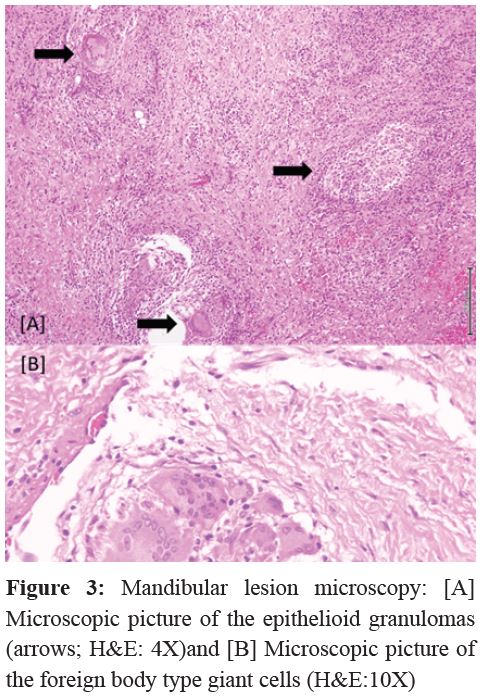
Mandibular lesion microscopy revealed tissue granulation with diverse inflammatory immune cells and multiple epithelioid granulomas containing foreign body type giant cells. Bony fragments, areas of necrosis, and calcifications were also noted. No malignancy was seen, hence, a conclusive diagnosis of a CGCG was made (Figure 3).
The patient attended multiple follow-up sessions at 1 week, 4 weeks, 3 months, and then annually. During follow-ups, he was regularly checked for healing of the wound, recurrence, infection, paresthesia, vitality of the nearing teeth, alteration in occlusion, facial asymmetry, tenderness, and his overall oral hygiene maintenance.
In the first follow-up, the patient complained of paresthesia, which then gradually reduced and completely disappeared in the subsequent followups. Overall, no untoward findings were observed, and the bone graft completely closed the defect with vital adjacent teeth. Three years follow-up study revealed no recurrence.
The incidence of CGCG is estimated to be very low, almost 0.0001%. Previous reports suggest that the mandible is frequently affected than the maxilla.7 In our study as well, it was observed that the lesion was located in the right mandibular angle and ramus with a proximal-mesial extension measuring 3 × 4 cm and spreading to involve the mandible right body with dissimilar and sclerotic boundaries, excluding the superior aspect region.
Many methods are established to treat CGCG. The commonly practiced and classical method of treating CGCG is by surgical intervention.8 The magnitude of this surgical intervention can range from curettage to en bloc resection of the lesion. This depends upon the type of lesion; whether it can be managed by simple curettage or an aggressive one which requires more intervention. Although, there are studies from other parts of Gulf, there are no studies reported in the Kingdom of Bahrain regarding CGCG and its surgical approach for treatment.
Conventional surgical approaches include either solely subjecting the lesion to curettage or curettage coupled with peripheral osteotomy with results of no recurrence. Similarly, lasers or cryoprobes are employed for the thermal sterilization of the margins of the lesions. Aggressive CGCG has sometimes been met with radical resection surgeries6 and although, the procedure is justified, recurrence cannot be denied, which might accompany with serious facial mutilation and tooth loss.
Pediatric cases warrant a conservative attitude to treat CGCG to avoid any longterm developmental defects. Osteoclastic activity was inhibited by steroids and calcitonin. Injecting equal parts of 0.5% bupivacaine then triamcinolone-acetonide (10 mg/mL) into the lesion for 11 weeks is proved to improve the condition. The approach has been contraindicated in immunocompromised patients and in conditions, such as diabetes mellitus and peptic ulcers.8-10
Treatment using calcitonin 200 U/spray one or two times daily (nasal) was testified as effective and safe. However, patient compliance was poor due to extensive duration of the treatment. Radiation treatment is a complete contraindication, as it may cause malignancy.8, 11 Interferon alpha and corticosteroid therapy are the latest treatment options. Recurrence of CGCG is more common and is observed in 46% cases. It is documented that recurrence rates of CGCG range from 11% to 49% for curettage alone and 72% for aggressive lesions.9, 10
In the case at hand, conservative approach of bone grafting was performed after enucleation of the lesion and defect location debridement. After operation, the inflammation and paresthesia gradually subsided over the first 4 weeks and it was promising to see the patient not inflicted with facial asymmetry, loss of teeth, abnormality of the mandible, or recurrence of the lesion. Bone grafting inclusion for treating CGCG should be further assessed to evaluate the active usage of this modality to reduce the persisting defects after conventional surgical interventions.
CGCG is a moderately exceptional benign lesion of a variably aggressive in nature or occasionally aggressive bony lesion. It must be ruled out in patients with former dental procedures that present later with mandibular swellings. Thorough clinical/ medical history and physical scrutiny are essential, along with the use of the necessary laboratory and imaging diagnostics. Histopathology biopsies are crucial in confirming the CGCG and in ruling out other, possibly-malignant, differential diagnoses. Recurrence of CGCG is well reported, and thus, advised for follow-up. Further, testing of the conservative approach for grafting the affected bone is recommended.
The authors of the study have no conflicts of interest to declare.