
Journal of the Bahrain Medical Society
Year 2020, Volume 32, Issue 3, Pages 1-8
https://doi.org/10.26715/jbms.32_2020_3_1Moutasem Al Mashour1*, Badriya Toorani2, Nada Al Mansoori3, Shaker Asheeri4, Owais Ahmed5
1Consultant, Anesthesia and Pain Management, Salmaniya Medical Complex, Manama, Bahrain
2Consultant, Orthopedic Spine Surgeon, Salmaniya Medical Complex, Manama, Bahrain
3Consultant, Anesthesia Department, Salmaniya Medical Complex, Manama, Bahrain.
4Chief Resident, Orthopedic Department, Salmaniya Medical Complex, Manama, Bahrain
5Chief Resident, Anesthesia Department, Salmaniya Medical Complex, Manama, Bahrain
*Corresponding author:
Moutasem Al Mashour, Consultant, Anesthesia and Pain Management, Salmaniya Medical Complex, Manama, Bahrain; Email: moutasem73@hotmail.com
Received date: April 17, 2020; Accepted date: July 20, 2020; Published date: September 30, 2020

Background: Sickle cell disease patients have a tendency for vaso-occlusive attacks involving their bones. Osteonecrosis results in infarction of the articular surfaces and heads of long bones, leading to chronic joint pain, significant interference in functioning and quality of life. Intraarticular Botox injection is safe andreduces chronic pain while patients’ mobility.
Objective: The study aimed to evaluate the symptomatic change and its duration after intra-articular Botox injection, in sickle cell disease patients with chronic pain.
Methods: Sickle cell disease patients with chronic joint pain observed at Salmaniya medical complex were included. Patients were injected with Botox intraarticularly and followed up for a year.Symptomatic parameters were assessed at every follow- up, raw data collected was entered into Microsoft Excel spreadsheet were the numerical variables analyzed and graphs were created.
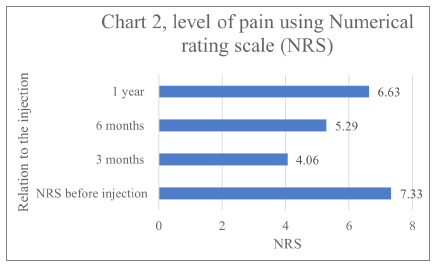
Results: Forty-eight sickle cell disease patients were included.Postthe intraarticular injection at 3 months, the level of pain according to, Numerical rating scale (NRS) reduced by 44.6 % (p-value <0.005) and 27.8%( p-value < 0.001) at 6 months and 9.54% ( p-value <0.01) at 1 year, and significant improvement of other parameters.
Conclusion: Intraarticular BoNT/ A injection provides an alternative treatment in sickle disease patients with good results in reduction of pain, improved physical function, mood, and sleep pattern lasting at least 6 months. Although a small scale study, the results suggest that BoNT/ A is an effective and safe treatment.
Keywords: Avascular Necrosis of Bone; Botulinum toxin; Chronic Pain; Injections; Intra-Articular; Sickle cell disease (SCD)
Sickle cell pain is the result of tissue ischemia caused by an occlusion of vascular beds with sickled erythrocytes creating hypoxia which can cause serious consequences, such as avascular bone necrosis(AVN) or tissue infarcts.1,2 This leads to chronic changes in the bone resulting in chronic pain and disability.
The natural history of the development of adult-onset osteonecrosis in patients who have sickle cell disease is currently unknown,3 as very few such patients have been followed by orthopedic surgeons before presenting for surgery because of pain.
The true prevalence of osteonecrosis in sickle cell disease is difficult to measure as of the small number of studies using sensitive methods of detection such as MRI consist mainly of international statistics and lack official national statistics. The overall prevalence of hip joint AVN is about 10 percent, with poor results after hip arthroplasty.3 The mean age of onset was 35 years and rare in the first decade of life.
The goal of therapy for patients with chronic pain is to improve functional capability while decreasing the level of pain.4,5
Health professionals are reluctant to prescribe opioids due to stigma with addiction and side effects.6 There is widespread fear of drug dependency when the painful crisis is managed with opioids. However, there has been no scientific evidence to support this assertion.7 Systemic analgesics is considered as oral analgesics have limited pain relief and may produce side effects and drug interactions.8
Alternative pathways for pain treatment such as interventional pain management has proven to be helpful in acute and chronic states. However, local joint injections of drugs such as steroids haven’t shown much improvement or long term benefit and is postulated as the most important cause of AVN with many side effects.9
The rationale of Botox injection intraarticularly for patients with chronic pain is to decrease the constant pain and improve functional capability. Botox was found to produce significant pain relief when injected into painful joints caused by inflammatory or noninflammatory disorders.10 With its use, a decrease in the number of analgesic drugs used to control pain episodes was observed thus alleviating the fear of the use of opioid drugs.
The primary aim of this study was to assess the symptomatic change after intra-articular Botox injection in the large joints in sickle cell disease patients, improvement of symptoms and duration of its effect.
The study was performed in AGU Arab Gulf University main hospital Salmaniya medical complex Bahrain. The study was conducted after reviewing existing literature on intra-articular use of Botox (BoNT-A) , its established use and safety.11 Forty-eight sickle cell disease patients between 16 to 60 years, with painful large joints for more than six months duration , localized pain at a specific joint and no improvement with physiotherapy were included. Patients with chronic pain conditions other than osteoarthritis, treated with corticosteroids in the study knee within 12 weeks or hyaluronic acid in the study knee within 24 weeks, previous treatment with Botulinum toxin with no benefit, diagnosed with myasthenia gravis, Eaton-Lambert syndrome, pregnant or non-ambulatory were not included.
Patients with sickle cell disease with chronic joint pain were assessed in the multidisciplinary clinic by chronic pain management consultant and orthopedic surgeon. Duration and degree of pain, and degree of joint damage was documented.
Treatment option of joint Botox injection was explained to the patient and informed consent was obtained. Post ethical approval from the institutional ethical committee the study was initiated
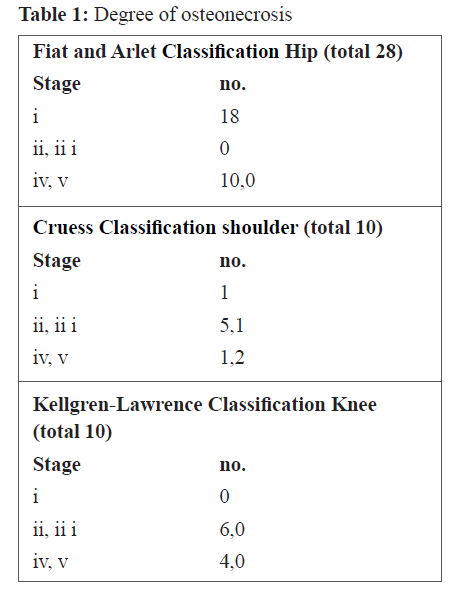
The orthopedic surgeons used various types of scores according to the joint involved to properly grade the degree of osteonecrosis. For the femoral head Ficat and Arlet classification of avascular necrosis which uses a combination of plain radiographs, MRI, and clinical features was used.12 The Kellgren, and Lawrence system classifying for the severity of knee osteoarthritis (OA) and Cruess. 13 Classification for the degree of shoulder osteonecrosis (Table1). 14
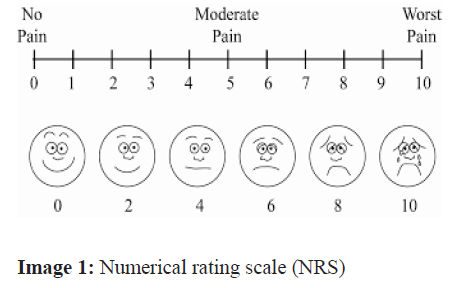
Before injection status: Baseline level of pain before the injection was recorded at rest subjectively by Numerical rating scale (NRS).
The patients were instructed to choose a number from 0 to 10 that best describes their current level of pain.(0 mean "no pain" and 10 mean "worst possible pain” (image 1).15
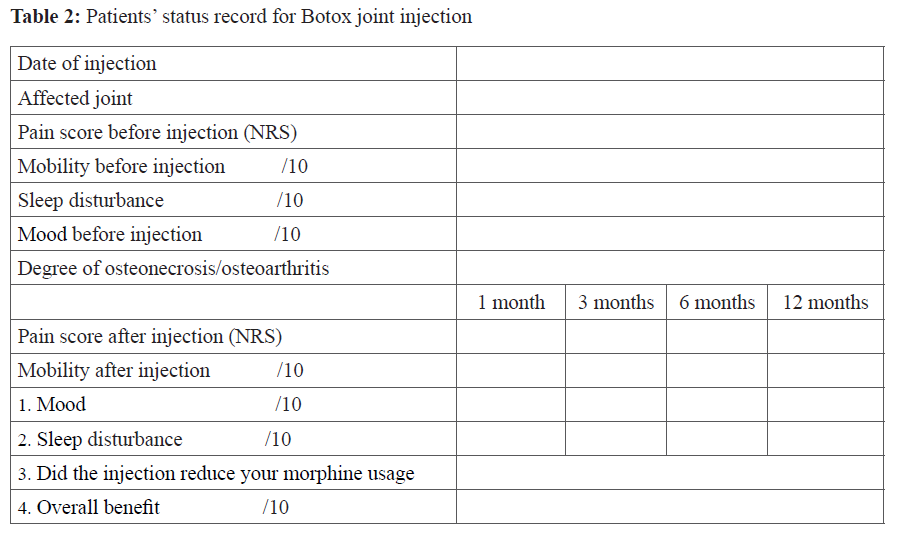
Patients status before and after the procedure were documented with a questionnaire incluive of ten questions. These were agreed upon by the different specialties involved in the study (pain management and orthopedics) (face validity) patients were asked about the clarity of the questions and their relevancy before adopting the questionnaire.The content of the questionnaire is presented in Table 2.
All raw data collected from the patients were entered into the Microsoft Excel spreadsheet program and all the numerical variables analyzed, and graphs were created. Statistics such as mean, standard deviation, and percentage were used to describe the participants’ demographic data.
After documenting the baseline condition of the patients they were moved for surgery. In the operation theater, patient was placed in supine position and under aseptic precautions the initial fluoroscopic image was taken. For the hip joint a 22 gauge 9 cm spinal needle was inserted anterolateral in the joint. For the shoulder joint a posterior approach was used, 2 to 3 cm inferior to the posterolateral corner of the acromion and directed anteriorly. For the knee joint a 22 gauge needle was inserted 1 cm above and 1 cm lateral to the superior lateral aspect of the patella. Intra-articular needle position was confirmed by fluoroscopic imaging and negative aspiration.0.2–1 cc iodinated contrast (Omnipague, Nycomed Inc., Princeton, NJ, USA) contrast media was first injected followed by a fixed dose of 100 units of botulinum toxin type A (Botox, Allergan Inc.) intra-articularly., Botulinum was diluted with 6 ml of normal saline.14 Post procedure the puncture site was covered with an antiseptic dressing. The patient was later discharged after confirming the absence of side effects. They were asked to report to emergency in case of any complications. Patients were followed up over one year. Follow up was done on phone at 3 months,6 months, and one year.
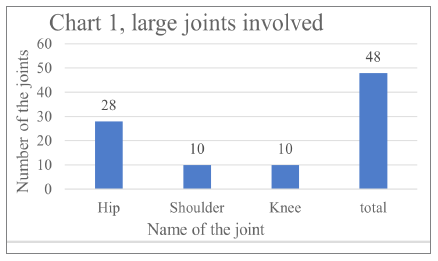
A total of 48 patients, 22 males and 26 females responded at 3 months, 47 at six months and 39 patients at one year. Three major joints were involved, the majority cases being the hip joint 58.3%. (chart 1).
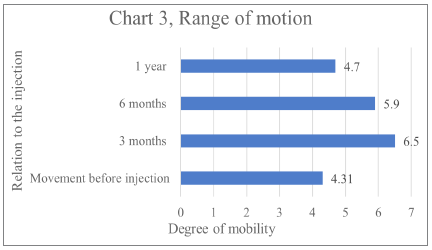
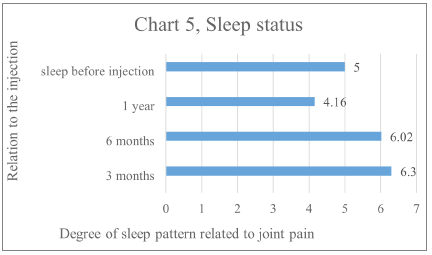
The average of pain NRS score before injection was 7.3 out of 10(mean 7.13, SD 1.52), the duration of pain before injection was more than 2 years, movement before injection was 4.3 out of 10 (1 is for no mobility 10 for a full range of mobility) (mean 3.9, SD 1.82), sleep disturbance due to joint pain before injection 4.9 out of 10(1 is for no sleep 10 for deep of sleep) (mean 4.5, SD 1.93), the mood before injection due to joint pain 5 out of 10(1 is a poor mood 10 for normal mood) (mean 4.7, SD 1.72) Regular Morphine usage due to joint pain and other causes was observed in 24 patients.
Pain: After the injection at 3 months follow up it was found that the patient’s level of pain according to Numerical rating scale (NRS) (0-10) scale reduced from average 7.3 to 4.06 (mean 3.35, SD 2.46), with reduction of pain 44.6 % the differences between groups was statistically significant (p-value <0.005) and 27.8% (mean 4.78, SD 2.45), at 6 months (p-value < 0.001) and 9.54%(mean 6.2, SD 3.18), at 1 year (p-value <0.01). (chart 2).
Joint disability : The patients were asked to grade their joint mobility at scale 1 to 10 At 3 months follow up mobility increased from average 4.3 to 6.5 51.1%(mean 6.9, SD 2.12), and 37.2 %(mean 5.4, SD 2.15), at 6 months and 9.3% (mean 4.3, SD 2.4), at 1 year. (Chart3).
Mood after the injection: The patients were asked to grade their mood at scale 1 to 10.At 3 months follow up patient’s mood improved from 5.1 to 6.4(mean 6.1, SD 1.8), with an increase of 25.41%(mean 5.7, SD 1.95), and 17 % at 6 months and reduced by 1.9% (mean 4.7, SD 2.57), at 1 year. (chart 4).
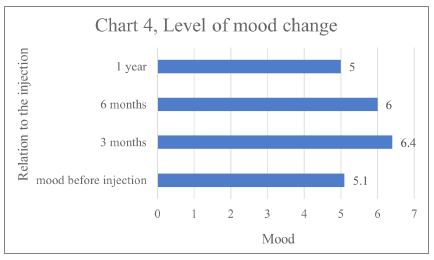
Mood after the injection: The patients were asked to grade their mood at scale 1 to 10.At 3 months follow up patient’s mood improved from 5.1 to 6.4(mean 6.1, SD 1.8), with an increase of 25.41%(mean 5.7, SD 1.95), and 17 % at 6 months and reduced by 1.9% (mean 4.7, SD 2.57), at 1 year. (chart 4).
Sleep after the injection: The patients were asked to grade their sleep status and relate it to the joint pain at scale 1 to 10. At 3 months follow up it was average of 6.3 (mean 5.9, SD 1.85), at 3 months and 6.02 (mean 5.8, SD 1.8), at 6 months and 4.16(mean 4.79, SD 2.53), at one year (chart 5).
For the question did the injection reduce your morphine usage, 16 (33.5%) patients answered affirmative.
After considering the dropouts, the total number of patients was38. We found, at 3 months follow up, patient’s level of pain reduced from average 7.3 to 4.06 with reduction of pain of 44.6 % and 39% at 6 months and 36% at 1 year.
Joint mobility at scale 1 to 10, After the at 3 months follow up it was found that the level of mobility increased from average 4.3 to 6.5 with an increase of mobility by 51.1% and 33% at 6 months and 11% at 1 year.
Mood after the injection at 3 months follow up improved from average 5.1 to 6.4 with an increase of 25.41% and 21% at 6 months and by 6.1% at 1 year.
Sleep after the injection, at 3 months follow up it was 35% and at 3 months and 30% at 6 months and 11% at one year.
And regarding the answer to the question did the injection reduce your morphine usage? 15 patients answered yes it did 42.11%.
The Joint Committee on Accreditation of Healthcare Organizations (JCAHO) in March 1999, approved standards for assessment and management of pain for inpatients and outpatients These standards stress that patients have a right to appropriate assessment and management of their pain. In 2000, JCAHO began to determine institutional compliance with pain management through interviews with patients, families, and clinical staff and review of pain-related policies and procedures.
Inadequate treatment of pain, new treatment standards, and increasing patient awareness of treatment alternatives all emphasize the need to improve the management of sickle cell chronic pain and decrease the number of analgesic drugs used to control pain episodes thus alleviating the fear of the use of opioids.
Botulinum toxin (Botox) is a neurotoxic protein produced by the bacterium Clostridium botulinum. It binds to the presynaptic cholinergic terminal and inhibits the release of acetylcholine and thereby blocks neurotransmission at the motor endplate15 (i.e., functionally deactivating the neuromuscular junctions by chemo-denervation). There are seven types of botulinum toxin,16,17 reviews summarize our current understanding of joint pain and various mechanisms contributing to it. 18
The joints are innervated with articular nerves that contain A-delta, A-beta, and C-fibers.
When the drug is injected into the closed capsule of the joint it causes denervation of the sensory nerves supplying that specific joint and thus confined to joint. Osteoarthritis pain is usually triggered by movement and load bearing. 19 It can also be experienced at rest and night. Being unpredictable, it is difficult for patients to take part in planned activities. Pain can be dull and aching, punctuated by intermittent, more intense episodes. People with osteoarthritis are at risk of falls due to pain, joint instability, altered gait, aging, and medication use, Between 31% and 41% of people with OA experience anxiety, compared with around 17% for all types of anxiety in the older adult general population.
BoNT/A is an effective treatment for painful movement disorders, spasticity, myofascial pain, and conditions with increased muscle tone, abnormal posturing, and pain and its safety also in repeating its injection in the joint according to Mahowald et-al.20,21
The rationale of Botox injection intraarticularly for patients with chronic pain is to decrease the pain and improve functional capability. BTX was found to produce significant pain relief when injected into painful joints caused by inflammatory or noninflammatory disorders.22
Botox injection according to many studies has an effect of 6-12 months is a good solution. Intraarticular Botox injection had been proven to be safe with good results in the reduction of pain and benefited patients in mobility to both sickle cell disease patients and none sickle patients.
The natural history of the development of adult-onset osteonecrosis in patients who have sickle cell disease is currently unknown,23as very few such patients have been followed by orthopedic surgeons before presenting for surgery because of pain. Because most adult patients with sickle-cell disease currently have a long life expectancy, with appropriate medical treatment, it would be beneficial to know the natural history in these patients.
Involvement of the femoral head osteonecrosis is common in sickle cell disease patients, as a consequence of infarction of the articular surfaces and heads of the long bones, those with frequent painful crises are at the highest risk. The overall prevalence is about 10 percent with poor results after hip arthroplasty.23
The diagnosis of femoral head osteonecrosis was made with the use of anteroposterior and lateral plain radiographs or magnetic resonance imaging, Magnetic resonance imaging was not used on a routine basis before 1985.24 However, between 1985 and 1987, magnetic resonance imaging was used as part of the initial evaluation. All magnetic resonance images were obtained with a 1.5-T superconducting unit, the diagnosis of osteonecrosis on magnetic resonance imaging was made based on band-like abnormal signals and band-like hypointense zones on T1-weighted images.25
Osteonecrosis was graded according to the method of Steinberg et al .26,27 Radiographic progression was defined as an advance in the Steinberg stage or progressive collapse. The extent of the osteonecrosis was quantitatively assessed by digitizing the area of the femoral head that was occupied by bone with abnormal texture on radiographs, on magnetic resonance imaging, and expressing it as a percentage of the entire femoral head.
Inadequate treatment of pain, new treatment standards, and increasing patient awareness of treatment alternatives all emphasize the need to improve the management of sickle cell pain crises.28 The pain and radiographic evidence which correlated in some cases and other instances did not and there was no significant change in the X-ray appearance after BoNT/A injection.28
In our study, we aimed to evaluate the relationship between pain, and quality of life which proved from the results of a direct linear relationship. We depended on the patient’s verbal evaluation of pain degree by questionnaire simplified for all to comprehend which can be considered a draw point in the study as patient observer bias.
The therapeutic effect of the injection persisted after BoNT/A was injected intra-articularly for more than 3 months in NRS and in 27% of patients for 6 months, patients joint mobility improved at 3 months by 51.1% and 37.2 at 6 months.
Hence, the therapeutic effect of BoNT/A is transient rather than long-term. It is proposed to have another injection to maintain the therapeutic effect.
The results we got in our study corresponds with the other published studies in regard to therapeutic effect, duration of action, and safety.
There were some limitations in our study. This was an open-label clinical trial with non-randomized treatment allocation, which favors patient and observer bias.
Intraarticular Botox injection had been proven to be safe with good results in the reduction of pain and showed benefits in patients’ mobility in both sickle cell disease patients and none sickle patients.
It provides a new therapeutic option for refractory pain among patients with Osteonecrosis / Osteoarthritis, the results can be generalized to sickle disease patients with chronic joint pain and in patients in whom surgery is not an option. Nevertheless, the good results we got from this small group of patients’ a larger study population would confirm our results.
All authors declare no conflicts of interest or received funding from any person or authority.