
Journal of the Bahrain Medical Society
Year 2020, Volume 32, Issue 3, Pages 26-29
https://doi.org/10.26715/jbms.32_2020_3_4Alia Khalil Ebrahim AlRabia1*, Rameshchandra Nair2
1MBBS, General Physician, Shifa AlJazeera Medical Centre, Manama, Bahrain
2MBBS DORTH, Orthopedic Surgery, Shifa AlJazeera Medical Centre, Manama, Bahrain
*Corresponding author:
Received date: February 5, 2020; Accepted date: August 3, 2020; Published date: September 30, 2020

Legg Calve Perthes disease is a self-limiting disorder characterized by avascular necrosis of unknown etiology affecting the femoral capital epiphysis. Complete revascularization of the avascular epiphysis invariably occurs over a period of two years, and the need for treatment of Perthes disease may therefore be questioned. Most recently, it has been observed that the development of Perthes disease can be preceded by recurrent or prolonged transient synovitis (TS) of the hip joint. We present a case of a five-year-old girl who was brought to the clinic with a history of intermittent hip pain and a limp for over a period of nine months.
Keywords: Legg Calve Perthes Disease; Transient synovitis; Avascular necrosis; Supervised neglect
The management of Legg Calve Perthes disease (LCPD) involves an array of considerations. Initially described as an idiopathic interruption of the blood supply to the proximal femoral head, with most cases reported at ages 4-10 years of age, the condition may be part of a general disorder of growth with a higher incidence in underprivileged communities.1 It is worth mentioning that the prevalence of this disease was calculated at 1:100,000 in Bahrain during the 1990s.2 We describe a case of Legg Calve Perthes disease that followed after a prolonged asymptomatic period of nine months from the onset of the first episode of transient synovitis which resolved spontaneously. A similar case was described previously by Tadahiko et al wherein it was suggested that physicians should consider LCPD and carefully observe if joint effusion continues and or symptoms do not improve within four weeks.3
A five-year-old Indian female was brought by her parents after she complained of left hip pain and a limp for ten days. She did not suffer from any medical illnesses, was born with a normal birth weight (2.75 kg) via normal vaginal delivery, attained developmental milestones at appropriate intervals, was well-built and nourished, with an unremarkable past surgical history and no history of any kind of injury. Family history was unremarkable for such a condition. The patient had suffered a similar attack of pain approximately nine months ago, for which she was evaluated by a physician in her country, and where, according to her parents, a plain hip x-ray was taken (no records of her visit were provided however).
Upon presentation, she appeared to have an antalgic gait. Inspection revealed apparent left limb lengthening, and no visible scars or sinuses on the hips. There was marked global restriction of movement of the left hip, with active and passive movement of the hip eliciting pain and muscle spasm. She exhibited the following passive ranges of hip motion: flexion 0 – 50 degrees, adduction 20 degrees, abduction in extension 0-30 degrees, internal rotation 25 degrees, and external rotation 30 degrees. The right hip maintained normal range of motion. A complete physical examination of the spine was normal, and she was neurologically intact. An array of investigations was explored in our center including serum Erythrocyte Sedimentation Rate (ESR) which was at a value of 20 mm/hour, C-Reactive Protein (CRP) was negative and a complete blood count (CBC) was normal. Coagulation profile, liver function tests, serum calcium, alkaline phosphatase, vitamin D3, thyroid profiles and phosphorus were all within normal values. More advanced laboratory and radiological investigations such as cytokine studies and Magnetic Resonance Imaging (MRI) were not performed due to limitation of resources at the center.
The diagnosis of LCPD was established based on history, physical examination, and x-ray radiograph (Figures 1 and 2) that clearly depicted the advanced features of the disease. The parents were reassured and sent home with an analgesia prescription. The hip pain and limp resolved spontaneously in a short period. A follow up appointment with the patient was scheduled for later, but her parents deferred to present due to COVID-19 related restrictions. The patient is currently asymptomatic and abiding by our medical advice to restrict physical activity. We plan to refer the patient for an MRI examination should symptoms arise again.
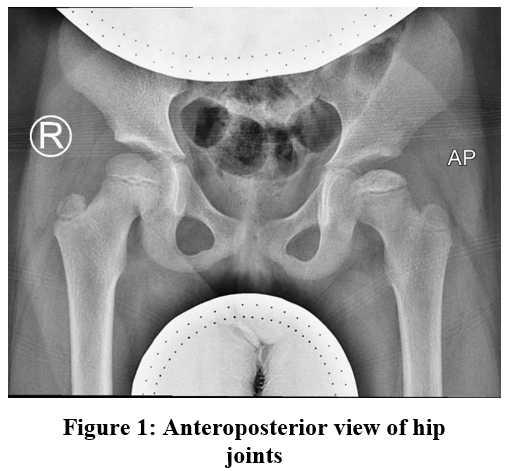 A plain radiograph of the hip (Figure 1, Anteroposterior view) showing increased density of the capital femoral epiphysis (CFE) of the left hip joint, with decreased height and medial joint space widening.
A plain radiograph of the hip (Figure 1, Anteroposterior view) showing increased density of the capital femoral epiphysis (CFE) of the left hip joint, with decreased height and medial joint space widening.
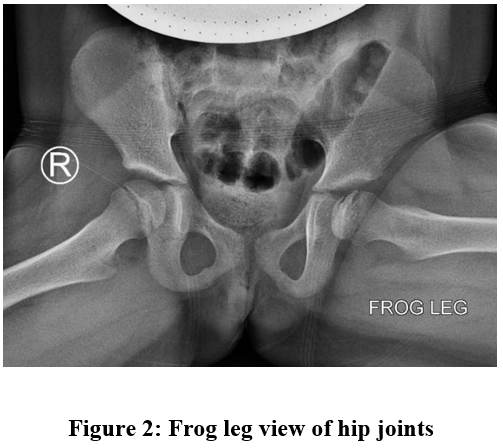 Figure 2, Frog leg view depicts a lateral subchondral fracture (Gage sign) running across the left femoral head.
Figure 2, Frog leg view depicts a lateral subchondral fracture (Gage sign) running across the left femoral head.
The treatment of Legg Calve Perthes disease emphasizes on the importance of preventing irreversible deformity of the femoral head. Extrusion of the femoral head appears to be a leading factor in the pathogenesis of the disease and its prognostication. Synovitis of the hip joint and articular cartilage hypertrophy contribute to the extrusion of the femoral head from the acetabulum.4 Herrings lateral pillar classification of the capital femoral epiphysis (CFE) published in 1992 effectively divides the extent of involvement of the femoral head into three groups, and we classified our patient to belong to group B of the classification, as more than 50% of the lateral pillar height was normally maintained. The other groups in the classification include group A (no involvement of lateral pillar) and group C (involvement of lateral pillar height >50%).5 According to the modified Herring classification, a B/C border group encompasses greater than 50% of lateral pillar height, narrow column (2–3 cm), or
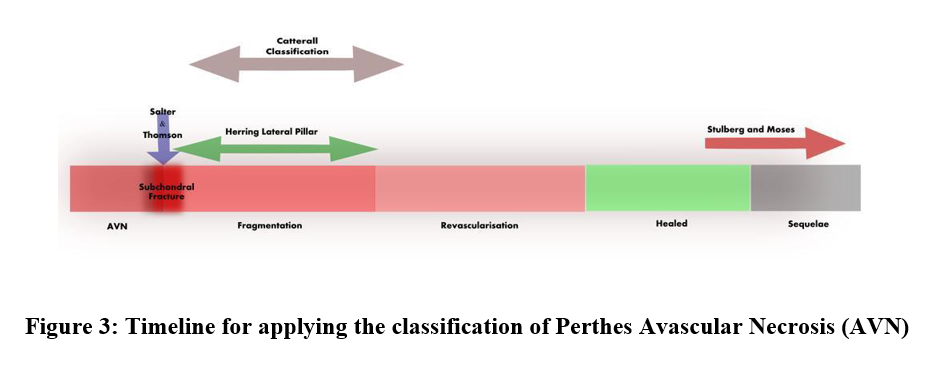
approximately 50% of pillar height maintained with poor ossification, or 50% pillar height maintained but depressed, relative to the central pillar.6 The application of the lateral pillar classification is based on the findings of early fragmentation of the femoral head.6 Above is a timeline (Figure 3) that depicts the appropriate time for the application of various classifications with concordance to the pathological stage of Legg Calve Perthes disease.
It was once thought that instituting treatment may not be needed in the pediatric age group with femoral head deformation specifically at the healing stage (since some of the cases do not present with pain and/or functional disability). The follow up of these children to adult life however clearly explains why treatment of LCPD during its active stage is necessary. More importantly, an initial plain radiograph of the hip joint with transient synovitis may appear normal. Several young adults with healed untreated LCPD develop clinical and radiological features of secondary degenerative arthrosis of the hip, which may pose a challenging problem in the future. Therefore, it is crucial to attempt to avoid this late complication of the disease.
The treatment of LCPD is not aimed at influencing the rate of revascularization but rather at performing serial clinical and radiological investigations to monitor the progression of the disease with the appearance of transient synovitis. It is crucial for recognizing the point at which intervention is necessary, be it conservative or surgical. Though the incidence of development of LCPD after episodes of transient synovitis (TS) is relatively low, occurring in 1-3% of individuals as once described,7 one may suspect the likelihood of the development of LCPD if TS does not resolve after two weeks, or reoccurs in children of 4 –10 years of age. Conferring to the literature, age is the main clinical prognostic factor. With our patient being less than nine years of age and noting the Herring lateral pillar category she belongs to (group B), her condition carries a fair prognosis. Hence, we decided to follow a treatment plan based on supervised neglect, minimal weight bearing, high impact activity restraint and re-evaluation after one month.
Unresolved or prolonged transient synovitis should raise the suspicion of the possibility of progression to LCPD in children of 4–10 years of age among other causes of hip pain. Patients who present with symptoms pertaining to transient synovitis should be subjected to follow up and reevaluation for a period of up to two years. As for the treatment options of early LCPD, supervised neglect is a feasible option for children who are of a younger age and those who belong to Herring groups A or B.
The authors declare they have no competing interests.
This work was not funded.
Not Applicable.
All documentations and data are available within the patient data system in Shifa AlJazeera Medical Centre.
We would like to thank Dr. Easwar T. Ramani MBBS, DNB (Orth.), MNAMS (Fellow in Pediatric Orthopedics, Deformity Correction and Spine and Scoliosis Surgery) for his useful suggestions and permission to use his timeline for applying the classification of Perthes disease for reference.