
Journal of the Bahrain Medical Society
Year 2020, Volume 32, Issue 3, Pages 40-44
https://doi.org/10.26715/jbms.32_2020_3_7Lateefa Almutawea1*, Jemila James2, Martin Corbally3, Arjun Dey4
1Pediatric Resident, Pediatrics and Neonatology Department, King Hamad University Hospital, Bahrain.
2Pediatric Registrar, Pediatrics and Neonatology Department, King Hamad University Hospital, Bahrain.
3Chief of medical staff/Consultant Pediatric Surgeon/Professor and Chairman, Department of Surgery, King Hamad University Hospital and Royal College of Surgeons in Ireland -Medical University of Bahrain.
4Neonatology Consultant, Pediatrics and Neonatology Department, King Hamad University Hospital, Bahrain, Email: acdey70@gmail.com; Mobile: 35948274.
*Corresponding Author:
Dr Lateefa Almutawea, Pediatric Resident, Pediatrics and Neonatology Department, King Hamad University Hospital, Bahrain, Email: latifa.almutawea@gmail.com; Tel. No.: (+973)-36306290.
Received date: May 13, 2020; Accepted date: September 10, 2020; Published date: September 30, 2020

Fetal volvulus without malrotation is a very rare neonatal surgical emergency. However, there is no reliable data on the incidence of fetal volvulus without malrotation. Fetal volvulus has variable degrees of presentation and survival rate of the fetus. Delay in diagnosis and timely intervention lead to increase in morbidity and mortality rates.
We report the case of a preterm neonate who was born at 30 weeks of gestation and was noted to have an intra-abdominal mass in utero. Intraoperatively, it turned out to be segmental midgut volvulus without malrotation.
Keywords: Fetal intestinal volvulus; Fetal midgut volvulus; Intrauterine volvulus; Prenatal diagnosis; Congenital midgut volvulus
Although the actual incidence rate of fetal volvulus is not known, the overall incidence of neonatal intestinal malrotation has been estimated as 1 per 6000 live births. The most serious consequence of malrotation is the volvulus. Midgut volvulus is a rare condition in which the small bowel and proximal colon twist around the superior mesenteric artery. This results in high-grade proximal bowel obstruction and vascular compromise of the intestine, which leads to infarction of the involved intestine. Midgut volvulus rarely occurs antenatally and is usually not lethal in utero.1
Prenatal diagnosis of midgut volvulus can be challenging as the antenatal clinical presentation is often nonspecific. Based on review of reported cases available in literature, clinical symptoms include decreased fetal movements, increased fundal height due to polyhydramnios, or a non-reassuring cardiotocography (CTG).2 Presence of polyhydramnios, intestinal dilatation, static abdominal mass, ascites and/or signs of fetal anemia on prenatal ultrasound assessment may indicate midgut volvulus.3 Doppler studies show an elevated peak systolic velocity in the middle cerebral artery due to severe fetal anemia, secondary to hemorrhagic ascites. The known complications of fetal volvulus reported in the literature include bowel perforation, hypovolemia, heart failure, pleural and pericardial effusions, and fetal demise.1,4 There were no specific clinical signs indicating volvulus without malrotation identified among the reported case series.5,6 Also, neither preoperative ultrasound nor radiological findings were suggestive of volvulus.
In this report, we present a preterm neonate who was reported to have a static abdominal mass with dilated intestinal loops on prenatal ultrasound. The postoperative findings were consistent with volvulus without malrotation.
A preterm female baby born at 30 weeks of gestational age with a birth weight of 1550 g to a para 2 unbooked mother who was referred for reduced fetal movements with non-reassuring CTG. A bedside ultrasonogram was done on admission which showed a fetal abdominal mass with dilated fetal intestinal loops with adequate liquor and no obvious congenital anomalies. The baby was delivered by emergency cesarean section with Apgar scores of 4 and 8 at 1 and 5 minutes, respectively. Due to premature birth with respiratory distress syndrome, the baby required intubation and surfactant administration, and was kept on mechanical ventilation. The abdomen was significantly distended from the time of birth. Abdominal ultrasonography was performed after stabilizing the baby, which showed hugely dilated colonic loops filled with feces and no air inside, with mild free fluid collection (Figure 1).
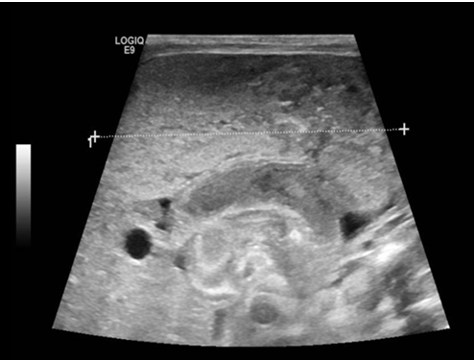 Figure 1: Ultrasonography of a neonate born at 30 weeks of gestation, showing a large intra-abdominal mass
Figure 1: Ultrasonography of a neonate born at 30 weeks of gestation, showing a large intra-abdominal mass
Extended workup was done including immunoreactive trypsinogen (IRT) test and cystic fibrosis transmembrane conductance regulator (CFTR) gene study for cystic fibrosis, which were reported as negative. Karyotyping was normal.
The patient was seen by the Pediatric Surgery team, and a trial of rectal wash was performed to relieve the fecal obstruction. As the abdominal distension persisted, an explorative laparotomy was performed on day 3 of life.
Intraoperative findings showed midgut segmental volvulus with thick tenacious meconium inside and 30 cm of gangrenous jejunum and ileum that was resected (Figure 2). There was no intestinal atresia or malrotation found. Histopathological examination concluded hemorrhagic infarction of the small bowel, consistent with volvulus.
 Figure 2: Postoperatively resected gangrenous ileal and jejunal loops measuring 30 cm in length
Figure 2: Postoperatively resected gangrenous ileal and jejunal loops measuring 30 cm in length
Postoperatively, the baby developed a right-sided pneumothorax which required insertion of a chest tube and mechanical ventilation for 10 days. Subsequently, the baby was weaned to continuous positive airway pressure (CPAP). Trophic feeding was introduced one week postoperatively, and the volume of feeding was gradually increased as tolerated. The baby remained clinically stable since then and was discharged at 6 weeks of age on full oral feeding and with satisfactory weight gain.
The baby was discharged from the neonatal intensive care unit and advised regular follow-up in the outpatient clinic for growth and developmental assessment.
Neonatal intestinal volvulus with malrotation is a well-known condition and has been reported in literature.7 There are also case series reported on primary volvulus without malrotation in the perinatal period, predominantly in infants born prematurely before 30 weeks gestational age.7 However, primary volvulus without malrotation is known to be a very rare event during the neonatal period.
Fetal volvulus results in increased morbidity and mortality. It is commonly associated with preterm birth and may present as a surgical emergency with a distended and discolored abdomen of the neonate. The etiology of fetal midgut volvulus without malrotation is unknown and the associated anomalies are rare. The few case reports available indicate that the possibility of fetal midgut volvulus should be considered when there is evidence of polyhydramnios, ascites, and a static abdominal mass with dilated intestinal loops on prenatal ultrasonography.3 The study by Mass et al7 is the only case-control study with 5 extremely preterm female infants weighing <600 g and gestational age of <26 weeks with small bowel volvulus without malrotation. Similarly, Billiemaz et al5 reported 6 females out of 7 affected infants with volvulus without malrotation. Our case study also involved a female infant. However, before considering gender as a potential risk factor for volvulus, we need more population-based data for better assessment.
The possible key factors responsible for prenatal volvulus without malrotation include stasis of bowel contents and longstanding subacute obstruction.6,8 Preterm neonates have immature intestinal motor function, which can lead to prolonged transition time and stasis of bowel contents. Considering this factor, one may speculate that extremely preterm infants are at a higher risk of developing volvulus without malrotation. Our case too presented a similar picture with the prenatal ultrasonogram showing dilated colonic loops filled with feces and thick tenacious meconium noted intraoperatively. Therefore, immature intestinal motor function could be the cause in our case as well.
Unfortunately, there were no disease-specific clinical signs suitable for discriminating volvulus without malrotation and necrotizing enterocolitis identified in the reported case studies. Any neonate presenting at birth or later in the neonatal period with acute abdomen should be evaluated for volvulus without malrotation and necrotizing enterocolitis. Prenatal diagnosis before the occurrence of irreversible intestinal ischemia may be difficult due to a lack of specific radiological or ultrasound features revealing the underlying strangulating obstruction, especially in the vulnerable population of extremely preterm infants.5,6 It has been suggested that immediate surgical consultation and prompt explorative laparotomy should be considered for preventing the complications of volvulus.
As with the review of previous case reports,5,6 the presentation of fetal volvulus could be variable. Molvarec A et al9 reported two cases of fetal midgut volvulus presenting as intrauterine intestinal obstruction detected on prenatal ultrasound. Another study reported intrauterine midgut volvulus without malrotation that presented as ‘coffee bean signs’ on the prenatal ultrasound due to meconium pellet.10 The literature also reveals that neither preoperative ultrasound nor radiological imaging was successful in detecting volvulus-specific features. Kornacki J et al11 reported a case of fetal midgut volvulus masquerading prenatally as ascites with fetal anemia as the Doppler ultrasound showed increased peak systolic velocity in the middle cerebral artery. Volvulus may cause vascular compromise that can lead to bowel infarction and eventual perforation of the necrotic bowel, which results in hemorrhagic fetal ascites and fetal anemia. Volvulus should be considered in the differential diagnosis when ultrasound imaging demonstrates dilated loops of bowel, especially in association with fetal ascites.2
In a recent case report by Monard et al,12 segmental small bowel volvulus presented with threatened premature labor. De Felice et al13 proposed an explanation on the relationship between intrauterine midgut volvulus and preterm delivery. They stated that acute fetal stress could activate both the fetal-placental adrenal and hypothalamic stress hormones, which could lead to premature uterine activity and preterm delivery.
Raherison R et al14 conducted a retrospective study and reported 10 neonates with prenatal intestinal volvulus without malrotation. The mean gestational age of their patients at birth was 36 weeks. None of their neonates had cystic fibrosis. Also, their study results suggested a good long-term outcome with prenatal volvulus although it is considered a life-threatening condition. In contrast, a case series published in 2016 by Sciarrone et al15 reported three out of eight neonatal volvulus cases to be positive for cystic fibrosis. The pathophysiology in such cases is thought to be due to viscous mucoid secretions obstructing the bowel lumen, hence, predisposing to volvulus. We investigated our case for cystic fibrosis, but the results were all negative.
Although fetal midgut volvulus is a rare condition, it is usually not lethal in utero. To date, there have been only 7 cases of intrauterine fetal demise caused by midgut volvulus reported in the literature.1
Ohuoba E et al16 performed a literature review on the survival rate of neonates with fetal intestinal volvulus and demonstrated that prenatal diagnosis and high index of suspicion affect the outcome decisively. Bawa and Kannan’s17 study demonstrated different outcomes of fetal intestinal volvulus based on the performance of prenatal scanning. In their review, one fetus identified with dilated bowel underwent prompt surgical intervention and survived, whereas the other succumbed with the postnatal diagnosis of volvulus where no prenatal sonography had been performed. They suggested that a single third trimester scan for fetal anomalies may be an effective strategy to reduce perinatal mortality.
Survival is influenced by the presence of other factors such as prematurity, volvulus evolving prenatally, size of affected bowel, and tolerance of surgery. Despite the presence of a few reported cases that were complicated by intestinal perforation, peritonitis, and bowel necrosis, the overall prognosis was good with eventual tolerance of feeds and weight gain.18
Postoperative short bowel syndrome is a known complication of bowel resection in general, but the remaining bowel length after small bowel volvulus resection is usually sufficient to allow normal feeding and growth.19 After a few precarious days of postoperative course of action, our baby remained stable, tolerated feeds without any signs of short bowel syndrome, showed satisfactory weight gain, and was discharged in stable clinical condition.
Despite improvements in prenatal diagnosis, the literature shows no studies comparing the outcomes of volvulus diagnosed prenatally versus postnatally. Further studies are required to differentiate between the outcomes of newborns diagnosed in the prenatal versus postnatal period.
Fetal volvulus is rare but can be a life-threatening pathology. Cystic fibrosis is commonly associated with this condition; however, it can be an isolated pathology as in this case. High index of suspicion with history, clinical and sonographic detection, prompt surgical intervention, and optimal postoperative care are the key factors for better outcomes with less morbidity.
Latifa drafted the initial manuscript of the case report. James J edited and wrote the final manuscript. Arjun and Corbally M supervised the aspects of the work.
None declared.
We are indebted to Dr. Emad Shatla, Dr. Minoosh Nasef, Dr. Raghu Shankar, and Prof. Imelda Lambert for their support in writing the manuscript.