
Journal of the Bahrain Medical Society
Year 2020, Volume 32, Issue 3, Pages 45-48
https://doi.org/10.26715/jbms.32_2020_3_8Shaikha Al-Doseri1*, Kanak Ganguly2
1Senior Resident Periodontist, Periodontics Doctorate (Sheffield), Dental and Maxillofacial Department, Bahrain Defense Force Hospital, Royal Medical Services, Kingdom of Bahrain.
2Chief Resident Periodontist, Dental and Maxillofacial Department, Bahrain Defense Force Hospital, Royal Medical Services, Kingdom of Bahrain.
*Corresponding Author:
Dr Shaikha Al-Doseri, Senior Resident Periodontist, Dental and Maxillofacial Department, Bahrain Defense Force Hospital, Royal Medical Services, Kingdom of Bahrain, Email: Shaikha.aldoseri4@gmail.com
Received date: June 21, 2020; Accepted date: September 10, 2020; Published date: September 30, 2020

Crown lengthening is performed to increase the length of the clinical crown for either restorative or esthetic reasons. Biological width is one of the important requirements to consider to avoid rebound of the gingival tissue. Indications for crown lengthening include excessive gingival display, short clinical crown, restorative procedure, and management of uneven gingival margins. In some cases, the gingival tissue does not retract to its full extent, leading to excessive gingival tissue display. This may affect the esthetics, necessitating crown lengthening. This article discusses the case of a 23-year-old female patient with excessive gingival display in the upper anterior segment that was treated with a crown lengthening procedure with osseous reduction.
Keywords: Crown lengthening; Gingivectomy; Surgical flap; Tooth crown; Wound healing
Crown lengthening is a procedure that is performed for either restorative or esthetic reasons. It involves increasing the length of the clinical crown for correction of excessive gingival display. Before initiating treatment, the clinician must consider the biological, functional, and esthetic aspects of each case.1 Consideration of the biological width of gingiva is one of the important requirements for avoiding rebound of the gingival tissue. Biological width is defined as the portion of the periodontal soft tissue that is attached to the tooth surface coronal to the crest of the alveolar bone.2 Invading this area can cause gingival inflammation or enlargement, clinical attachment loss, and bone loss. Surgical crown lengthening prevents such complications.3
Indications for crown lengthening include excessive gingival display, short clinical crown, restorative procedure, and management of uneven gingival margins.4,5 Contraindications for crown lengthening include smoking, thin periodontal biotype, inadequate band of the keratinized gingiva, periodontal disease with the loss of bone support, and presence and extent of caries.6
During treatment planning, multiple factors such as the smile line, crown-to-root ratio, position of the cementoenamel junction, width and thickness of the keratinized tissue, and health of the periodontium must be considered.7
The most common surgical approaches for crown lengthening include gingivectomy, apically repositioned flap, and apically repositioned flap with osseous reduction.6
Gingivectomy involves removal of excessive gingival tissue from an area with enough keratinized tissue and using it in gingival overgrowth cases or false pocketing. Apically repositioned flap is preferred when the width of the keratinized tissue is insufficient. In this technique, the gingival tissue is relocated to an apical position instead of removing it. Apically repositioned flap with osseous reduction is used to preserve the biological width, and it involves displacing the gingival tissue with removal of the alveolar crest bone.6
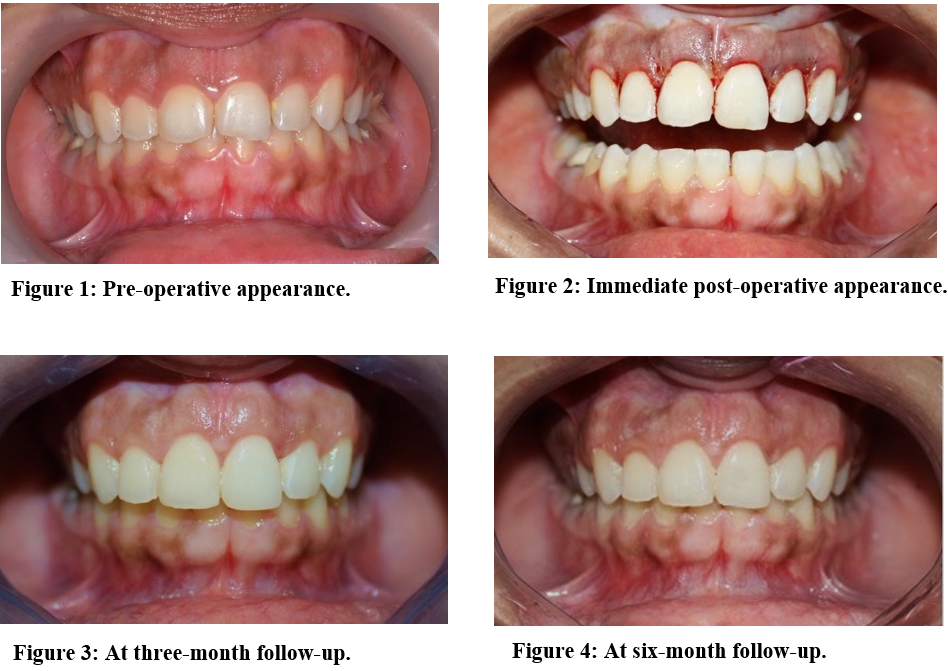
A 23-year-old female patient presented with an excessive gingival display or “gummy smile” in the upper anterior segment (Figure 1). She was concerned about the appearance of her teeth and gums when smiling. The patient’s dental history revealed that she had had an orthodontic treatment done 4 months ago, and she had noticed the persistent “gummy smile” after that treatment. She denied any medical illness.
On clinical examination, the soft tissue revealed the presence of generalized plaque-induced gingivitis, a thick gingival biotype, and the width of the gingival display to be 5 mm when smiling. Oral hygiene was not satisfactory. The basic periodontal examination revealed all the sextants to have a score of 2 except the upper anterior sextant which scored 1, with score 1 representing bleeding on probing and score 2 indicating the presence of calculus or plaque retention factors (in this case, it was calculus).
There was a significant change in the oral hygiene and a major reduction in gingival inflammation following regular oral hygiene education. Since the patient’s primary issue was the appearance of her smile, the best option for addressing this concern was surgical crown lengthening procedure.
After the stabilization stage of her oral health, the patient was deemed to be ready for the surgical procedure. A preliminary evaluation of the bone margins by bone sounding under local anesthesia revealed their proximity to the gingival margins. Additionally, the width of the keratinized gingiva was too small to be entirely sacrificed. Hence, the surgical procedure indicated was crown lengthening with osseous reduction using an apically repositioned flap. The procedure was performed under local anesthesia after obtaining a written consent from the patient. Bone sounding was repeated to precisely map the position of the crest of the alveolar bone. Then, an internal bevel incision was made 3 mm from the gingival margin, in a scalloped pattern following the anatomy of the upper six anterior teeth (teeth number 13,12, 11, 21, 22, and 23). This was followed by the second or intra-crevicular incision, after which the incised gingival tissue was removed. The third incision was made in the interproximal spaces to release the interdental papilla. Subsequently, a full-thickness flap was raised to allow bone exposure. After raising the flap, an osseous reduction of 3 mm was done using a large, round carbide bur with copious irrigation. External vertical mattress suture technique was used to stabilize the flap in an apical position using 4-0 Caprosyn suture (CovidienTM). Hemostasis was achieved, and post-operative instructions were given to the patient (Figure 2).
The patient was seen one week postoperatively for the assessment of healing, addressing any complications, and removal of the sutures. No complications were noted. She was recalled after one month and then after three and six months for follow-up. The healing, oral hygiene, and appearance were satisfactory at the one-month follow-up appointment. The follow-up after three months (Figure 3) was to evaluate the healing, esthetic outcomes, and patient satisfaction. The follow-up at six months was done to assess the stability of the soft tissue at the new level, and the esthetic outcomes again (Figure 4). Both the healing and esthetic outcomes were found to be satisfactory at three and six months’ follow-up (the gingival display while smiling was 1-2 mm). The patient was pleased with the esthetic outcomes. The upper central incisors were restored with direct composite restorations to recreate a symmetrical appearance of both and improve the esthetics (Figure 3).
The common reasons for the crown lengthening procedure can be either esthetic or restorative. The esthetic component is often the patient’s main issue, and it usually involves “gummy smile,” which may be associated with short clinical crowns (Figure 1). The other common reason for performing crown lengthening pertains to creating enough space for restoration to avoid invading the biological width that could result in periodontal complications.3,5
Soft tissue considerations such as the gingival biotype and the extent of keratinized gingiva determine the type of surgical technique to be used. The gingival biotype can be classified as thin and thick biotype. The thin gingival biotype is susceptible to inflammation and recession. The thick gingival biotype is dimensionally more stable during remodeling when compared to the thin biotype but is more prone to rebound, necessitating bone removal.8 The case in this report was a thick biotype, and the soft tissue remained dimensionally stable during the healing phase due to the surgical technique used (Figures 3 & 4).
Before proceeding with the surgical treatment, the clinician must study the complete dental history of the patient and perform a comprehensive clinical examination and obtain radiographs to formulate the best treatment plan. During treatment planning, the clinician must also consider the wound healing, esthetic outcome, complications, and patient satisfaction. His decision regarding the procedure should be based on the indications and contraindication of the case, following comprehensive examination and planning.4,6,9
The surgical technique used in this case was crown lengthening via apically displaced flap with removal of osseous tissue. The aim was to reduce the extent of gingival display and maximize the clinical crown height of the upper anterior teeth. The reason for using this technique was to avoid rebound of the gingival tissue to its original position. Hence, bone removal and re-contouring were often required to help re-establish the biological width. Ideally, the planned crown margin should be at least 3 mm away from the alveolar crest.7 In this case, after elevating a flap and exposing the bone, 3 mm of bone removal was enough to re-establish the biological width into a new position and achieving an esthetically pleasing result.10,11 The final follow-up of this case at six months (Figure 4) was to assess gingival tissue stabilization and maturation after healing and to ensure that the biological width re-establishment happened between 3-6 months. There was no difference in the result between three and six months.7,11,12
There is always a risk of complications during any procedure. The common complications associated with crown lengthening surgery are root sensitivity, transient mobility, and tissue rebound.4 The clinician must anticipate and manage these complications. For example, in case of root sensitivity, the clinician must apply desensitizing agents to the sensitive teeth and prescribe a desensitizing toothpaste or mouthwash to the patient.
The results of this case were satisfactory as the appearance in terms of the “gummy smile” was improved and the patient was pleased with the outcome.
Crown lengthening procedure should be considered in cases of excessive gingival display to enhance the esthetics. In this case, the esthetic result was satisfactory. For a successful treatment, comprehensive examination and treatment planning is essential, in addition to patient compliance specifically in terms of attendance and oral hygiene measures.