
Journal of the Bahrain Medical Society
Year 2017, Volume 29, Issue 3, Pages 28-34
https://doi.org/10.26715/jbms.29.3.2017.40aOlisova OY1, Tepljuk NP1,, Grabovckaya OV1,, Belkharoeva RK1,, Hubail AR1*,, Pinegin VB1,
1Department of Skin and Venereal Disease Hospital named after VA Rakhmanov, I.M. Sechenov First Moscow State Medical University, Moskva, 119992, Russia.
*Corresponding author:
Amal Hubail, Dermatology Resident, Department of Skin and Venereal Disease Hospital named after VA Rakhmanov, I.M. Sechenov First Moscow State
Received date: May 14, 2017; Accepted date: July 25, 2017; Published date: August 8, 2017

Abstract
The aim of this study was to highlight the importance of a diagnostic approach to photodermatoses, selectively review the literature of the past 25 years, and describe the modern nosology of photodermatoses, their clinical features, diagnosis, and treatment.
Photodermatoses are a non-life-threatening condition; however, can cause considerable suffering. Without treatment and preventive measures, symptoms gradually worsen over a number of years and become chronic.
Keywords: Photodermatoses, Polymorphic light eruption, Erythematous lesions, PUVA
Introduction
Sunlight induces a wide variety of dermatoses. The differential diagnosis is problematic because of the confusing nomenclature and classification. Polymorphic light eruption (PLE) is the most common endogenous photodermatoses, with a prevalence of 10%–20% in Central Europe, Scandinavia, and the United States of America.1 It occurs in 20% of southern Scandinavia, 10% of North Americans, and southern British, 5% of southern Australians; however, it is not observed among equatorial Singaporeans. The incidence increases with increase in distance from the equator.2 The polymorphic photodermatoses are quite rare in the indigenous population of the regions with a constant high intensity of solar radiation. It is likely to develop in the inhabitants of Northern latitudes, who come for a short winter vacation in a tropical country. However, the prevalence does not exist in Russia.
Case report
A 69-year-old patient presented to our practice, complaining of symptoms since she was 65 years old. At that time, the patient was exposed to sunlight after which she noticed the appearance of a pruritic rash. Since then, the symptoms have been on and off increasing in the spring or after short holidays abroad. For past 3 years, whenever symptoms appeared, she visited a dermatologist who gave her oral antihistamines and topical steroid creams, mild improvement was observed after the visit. The symptoms generally appeared in the beginning of spring and started to improve by autumn. The dermatologist then gave her the diagnosis of either sarcoidosis or xanthelasmatosis. However, after she presented to our practice, we excluded these two and diagnosed her as having polymorphic photodermatoses based on the clinical picture and histological examination.
Table 1: Data collection of the patient
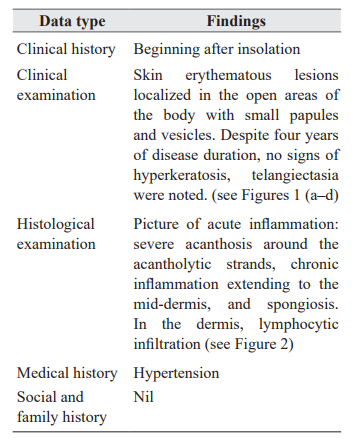
Figure 1, a-d: Patient’s rashes on presentation
Diagnosis
The diagnosis of PLE can be established on the basis of clinical and laboratory data. Photoprotection tests include either a monochromator phototesting or a provocation test. Monochromator measures the minimal erythema dose (MED) by employing a filtered high-pressure xenon arc lamp, which delivers ultraviolet (UV) and visible light across the solar spectrum on the back of the patient. MED lower than normal indicates abnormal photosensitivity.3 Phototesting is beneficial to give us an idea of the differential diagnosis and the responsible UV action spectrum.4
Photopatch test can be done in a case of suspicion of contact or photo contact allergy. The most common allergens are sunscreens and nonsteroidal anti-inflammatory drugs.5 To exclude the diagnosis of lupus erythematosus in some cases, a biopsy and immunofluorescence study may be needed to determine the titer of antinuclear antibodies and antibodies to the nuclear antigens Ro/SS-A and La/ SS-B.
Figure 1 (a-d): Patient’s rashes on presentation
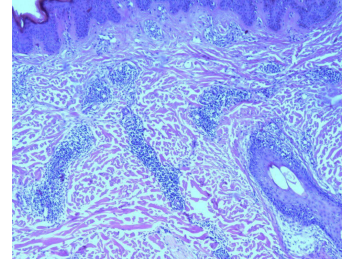 Figure 2: Histopathology slide
Figure 2: Histopathology slide
Blood and urine laboratory tests, including serological test (antinuclear, SS-A, and SS-B antibodies levels), as well as direct and indirect reaction immunofluorescence, may be needed to facilitate differential diagnosis. Also, we may need to check for porphyrins in the plasma, erythrocytes, and urine to rule out porphyria.5
In the present case, the patient underwent a full blood count including lipid profile, which ruled out xanthelasmatosis. Using an established 5-point scale, monochromator phototesting showed MED grade as ++, which was the bright red color with slight edema on palpation. A sample biopsy of the skin lesion showed histopathologically the presence of superficial and deep infiltrates as mentioned above. Most commonly, in such conditions, they are perivascular dermal inflammatory infiltrates that mainly constitute T lymphocytes—CD4+ and CD8+ cells. There was also an absence of deposition of acid mucopolysaccharide in the dermis. Upper dermal edema and spongiosis may be found.6 Provocative phototesting and photopatch testing were not performed, as the diagnosis was confirmed by clinical appearance and investigations performed already. The skin biopsy also did not show any evidence of sarcoidosis, chest x-ray, and pulmonary function test were performed to rule out the previously sought provisional diagnosis of the same.
Differential diagnosis
PLE should be differentiated from lupus erythematosus, especially in the presence of plaques. Cutaneous lupus erythematosus, discoid, and disseminated lesions are usually localized on the areas not specific to polymorphic photodermatoses.
Other differential diagnoses include actinic prurigo, which is a chronic idiopathic photodermatosis. It is characterized by, porphyria, other photodermatoses, toxicoderma, Jessner lymphocytic infiltration, sarcoidosis, and eosinophilic granuloma of the face. Also, photosensitive atopic dermatitis, seborrheic dermatitis, exudative erythema multiforme etc. are skin diseases that worsen or are triggered by sunlight/UV light.5
Treatment
Treatment is mainly aimed to minimize sun exposure, especially between 11 am and 3 pm, regular usage of protective clothing and broad-spectrum sunscreens blocking long-wave UVA radiation, particularly those which contain avobenzone, titanium dioxide, and zinc oxide.5 As UV rays remain throughout the day, UV protection should be recommended for the entire day and should be applied thickly and evenly throughout the year in all seasons.
Potent to very potent corticosteroids can be applied daily, especially in holiday-only PLE from a day before till the third day after the holiday.7 Few studies have shown that symptomatic treatment using topical glucocorticosteroid for 3–14 days has relieved itching and reduced the rash. However, controlled trials proving their efficacy are not available.8 Controlled trials have been conducted to study the use of antimalarial drugs such as hydroxylamine and chloroquine. However, these drugs were observed to have fewer benefits due improper patient blinding and their accumulation in the body and causing irreversible damage to the retina. Therefore, all patients taking antimalarial drugs for more than a year should be examined by an ophthalmologist for retinopathy.9
The method of psoralens UVA (PUVA) therapy can be highly effective; however, it is unclear whether the reasons for the effect are actions of T lymphocytes or changes of the epidermis in the form of thickening of the stratum corneum and increasing the content of melanin. Sessions are conducted three times a week for 4 weeks. The chemotherapy cycle is repeated every spring; however, after 3–4 years the need for it usually disappears.10 Prophylactic phototherapy improves the skin tolerance of patients to sunlight, prevents the development of relapses in the summer, and reduces the severity of the clinical manifestations.
In the comprehensive treatment of polymorphic photodermatoses, antioxidants (β-carotene) are included in literature; however, the lack of evidence makes it difficult to come to an unambiguous conclusion about the appropriateness of their use. In severe cases; however, immunosuppressive drugs such as azathioprine or cyclosporine can be used as an alternative therapy.11
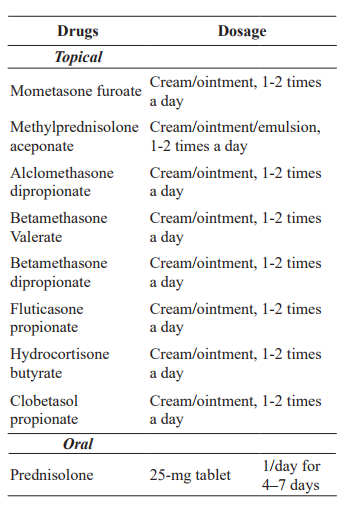
The recommended topical glucocorticoid preparations available are shown in Table 2.12
The patient was treated as follows:
1. Photoprotection regimes as outlined above
2. PUVA therapy; patients received narrow band UVB 311, three times a week for a total of 12 sessions
3. Hydroxychloroquine sulfate 200 mg one tablet per day for 2 weeks
4. Antioxidants: carotenoids in alpha-tocopheryl acetate 100 mg for 1 day, methionine 0.25 g three times a day for 1 day, xantinol nicotinate 0.15 g 3 times a day
5. In the acute phase: Mometasone furoate two times per day
Table 2: Recommended topical glucocorticoid preparations
 Outcome and follow-up
Outcome and follow-up
PLE is the most common of the idiopathic photodermatoses. Adherence to treatment and preventive measures provides successful symptom control and good long-term prognosis unless the patient does not adhere to strict sun precautions in the following years. That is why the prevention of polymorphic photodermatoses plays a crucial role in controlling this disease. Incidence increases with distance from the equator. That is thought to be due to the higher proportion of UVA further from the equator, as UVB suppresses the immune response in the skin and UVA tends to provoke the rash.12Age of onset is usually 20–40 years; however, this does not exclude its occurrence at a later age, as in cases with our patient, therefore, along with laboratory and histological analysis, a careful collection of anamnesis of the patient played a crucial role in the diagnosis.
If the patient fails to get the appropriate treatment or there is failure of compliance, there may be unwanted psychological effects due to embarrassment of the appearance of the skin, necessity to remain indoors most of the time, inability to perform hobbies such as swimming, medical expenses of treatment and follow-up, and having to change or discontinue occupation.13
Follow-up of the patient showed great result outcome, the rash decreased significantly and the itch was not present anymore.
Discussion
UV radiation is a component of the spectrum of solar radiation reaching the earth’s surface along with visible light and infrared radiation. The proportion of UV rays in the solar spectrum is 10%, visible light is 40%, and infrared radiation to 50%. UV rays on the scale of electromagnetic waves occupy an intermediate position between X-rays and visible spectrum. UV rays are divided into three ranges.14
Lack of UV light can cause children to develop rickets due to a lack of vitamin D, disorders of calcium-phosphorus metabolism, and reduced activity of protective systems of the body primarily the immune system.
In response to UV radiation in the skin, the stratum corneum absorbs approximately 70% of UVB rays in which 15% reaches the dermis. On the other hand, UVA rays do not cause sunburn. There is a cumulative effect, leading to changes such as skin flushing and the presence of photodyskeratotic cells, decrease in the number of Langerhans cells, and changes in their morphology and functional state.9 Excessive exposure has been linked to increased risks of skin diseases and cancers, mainly melanoma, and accelerates the skin photoaging process. In the eye, acute photokeratitis and photoconjunctivitis may occur, while chronically sun exposure may cause pterygium, cataract, or squamous cell cancer of the conjunctiva. It has also been seen that UV exposure alters the body’s immune response by changing the activity and distribution of the cells and hence, suppresses the immunity, therefore, increasing the risk of infection. Lastly, it can increase the thermal effects on the body leading to heat strokes (see Figure 3).15
Photosensitivity dermatoses are a large pathogenetically diverse group of diseases caused by an abnormal reaction to sunlight, usually the UV component, which develops in minutes, hours, or even days after exposure and lasts for weeks or months. The differential diagnosis is problematic not only because of the similar phenotypes but also because of the confusing nomenclature and classification. Photodermatoses may be divided into four groups (see Figure 4).16 In 1900, a Danish dermatologist, Rasch, proposed the term PLE for a description of two cases—the clinical picture that was simultaneously consistent with solar eczema and prurigo.9 PLE is a delayed reaction of the skin to sunlight that resolves without scaring. It is called polymorphic because it has several variants. Polymorphic photodermatoses have extensive morphological variants: lichenoid papules, prurigo, polymorphous erythema, granuloma annular, and eczematous.17
Figure 3: Types of waves reflecting on earth
Polymorphic photodermatoses affect men and women of all ages. Women are more affected than men. It usually occurs fair-skinned people with skin types (Fitzpatrick skin types I-IV).
PLE tends to occur during spring and early summer, and when the person’s exposure to sunlight increases. Repeated episodes are less likely as the summer progresses. However, the rash often recurs each year after the first incident.18 It is localized in sun-exposed areas of the body—on the neck, chest, shoulders, forearms, legs, more rarely on the face, and body. The duration of exposure, sufficient for the appearance of the rash, is usually from 30 min to several hours. Although, in the absence of reexposure, it may take up to 7–10 days.19 The most characteristic lesions are the papules, which are 0.2-1 cm in size, and pink, red in color. These are located on an erythematous background, which usually has a tendency to merge, then turn into papulovesicular elements and platelets. Rashes on the skin can be mixed or occur alternately (first papules then vesicles) which makes pruritus and solar eczema as the clinical variant of polymorphic photodermatoses. It is also characterized by the phenomenon of adaptation (hardening)—decrease of symptoms after repeated patient’s stay in the sun for a short period. This phenomenon is due to the tolerance of the skin to sunlight. Therefore, rashes appearing in spring or early summer do not recur in the future. In a few years, in some patients, the severity of relapses may decrease .3
Figure 4: Classification of photosensitivity diseases
The etiology of PLE is not entirely known, and it is likely to be multifactorial. The immunologic pathogenesis of PLE is confirmed by the study of biopsy samples of PLE lesions. The CD4 subtype of T cells, usually seen very early after exposure, is replaced by CD8 lymphocytes in 72h after irradiation. In general, this finding corresponds to type IV delayed type of hypersensitivity mechanism.5 It has been shown that there is a significantly decreased neutrophil infiltration in PLE skin, which is mainly due to reduced expression of tumor necrosis factoralpha, IL-4, and IL-10 in the UVB-irradiated skin.6
UV exposure is usually suppressed by the release of immunosuppressive cytokines from keratinocytes. It has been found that 17β-estradiol somehow prevents this response, leading to polymorphic photodermatoses. This theory explains the increase in its prevalence in adult women and tends to decrease after menopause.20
In the development of polymorphic photodermatoses, genetic predisposition and the intensity of the initial UV irradiation play a principal role. Approximately 50% of patients with polymorphic photodermatoses are sensitive to UVB radiation, and 75% to UVA, counting that in each of the cases is approximately 25% of those who are sensitive to both types of radiation.
In 1942, it was concluded that production of photoinduced skin antigens due to inherited abnormalities in the normal reduction of UVinduced immunosuppression leads to increased reaction to photoantigens and development of clinical damage.13
Genetics plays a role among patients with polymorphic photodermatoses, especially in the syndromic families (12%–46%). On supervision, 15% of monozygotic pairs of twins, compared to 5% of dizygotic pairs, had polymorphic photodermatoses.3
Learning points:
1. Prevention is better than cure in photodermatoses generally.
2. Psychological assessment might be needed is severe types due to distress.
3. Patient understanding of the nature of the condition is vital for better prognosis.
4. Differential diagnoses have to be considered thoroughly and addressed in order to avoid confusion.
Conflict of Interest
None
1. Gambichler T, Al-Muhammadi R, Boms S. Immunologically mediated photodermatoses: diagnosis and treatment. Am J Clin Dermatol. 2009;10(3):169-80.
2.. Ling TC, Dawe RS, Gardener E, et al. Interventions for polymorphic light eruption. Cochrane Database Syst Rev. 2005;1:1-9.
3.. De Argila D, Aguilera J, Sánchez J, et al. Study of idiopathic, exogenous photodermatoses. Part II: Photobiologic testing. Actas Dermosifiliogr. 2014;105(3):233-42.
4.. Schornagel IJ, Guikers KLH, Van Weelden H, et al. The polymorphous light eruption–severity assessment score does not reliably predict the results of phototesting. J Eur Acad Dermatol Venereol. 2008;22(6):675-80.
5.. Ibbotson S, Dawe R. Cutaneous photosensitivity diseases. In: Griffiths C, Barker J, Bleiker T, Chalmers R, Creamer D, eds. Rook’s Textbook of Dermatology.9th ed. 2016. Wiley-Blackwell; 2016.
6.. Horkay I, Krajczar J, Bodolay E, et al. A study on cell-mediated immunity in polymorphic light eruption. Dermatologica. 1983;166(2):75-80.
7.. Man I, Dawe RS, Ibbotson SH, et al. Is topical steroid effective in polymorphic light eruption? Br J Dermatol. 2000;143(57):113.
8.. Boonstra H, Vanweelden H, Toonstra J, et al. Polymorphous light eruption: A clinical, photobiologic, and follow-up study of 110 patients. J Am Acad Dermatol. 2000;42(2):199-207.
9.. Murphy GM, Hawk JL, Magnus IA. Hydroxychloroquine in polymorphic light eruption: a controlled trial with drug and visual sensitivity monitoring. Br J Dermatol. 1987;116(3):379-86.
10.. Regan JD, Parrish JA. The science of photomedicine. Springer, US; 1982.
11.. Norris PG. Successful treatment of severe polymorphous light eruption with azathioprine. Arch Dermatol. 1989;125(10):1377-9.
12.. Khopkar U, Pande S, Nischal K. Handbook of dermatological drug therapy. New Delhi: Reed Elsevier India Publications. 2007:198-200.
13.. Stratigos A, Antoniou C, Katsambas A. Polymorphous light eruption. J Eur Acad Dermatol Venereol. 2002;16(3):193-206.
14.. Frain-Bell W, Mackenzie L, Witham E. Chronic polymorphic light eruption (a study of 25 cases). Br J Dermatol. 1969;81(12):885-96.
15.. World Health Organisation. Solar Radiation and human health. 1999; Available at: http://www.who.int/uv/resources/fact/en/ fs227toomuchsun.pdf. Accessed June 3, 2017.
16.. Bylaite M, Grigaitiene J, Lapinskaite GS. Photodermatoses: classification, evaluation and management. Br J Dermatol. 2009;161(3):61-8.
17.. Calzavara PPG, Venturini M, Capezzera R, et al. Photosensitive erythema multiforme and erythema multiforme-like polymorphous light eruption. Photodermatol Photoimmunol Photomed. 2003;19(3):157-9.
18.. Mayo Clinic Staff. Polymorphous light eruption. Available at: http://www.mayoclinic. org/diseases-conditions/polymorphous-lighteruption/home/ovc-20308891.Accessed June 3, 2017.
19.. Bhutani L. The photodermatoses as seen in tropical countries. Semin Dermatol. 1982;1(175):81.
20.. Aubin F. Why is polymorphous light eruption so common in young women? Arch Dermatol Res. 2004;296(5):240-1.