
Journal of the Bahrain Medical Society
Year 2018, Volume 30, Issue 1, Pages 45-51
https://doi.org/10.26715/jbms.1_26032018aDeyana Ditto1*, Taghreed Ajoor1, Manar Al-Khashram1, Tabassum Tayab1, Wafa Al Sharbati2
1Oral and Dental Health Services, Primary Health – Ministry of Health, Road 4025, Al Juffair 340, 12, Bahrain.
2Public Health Directorate, Ministry of Health, Bahrain.
*Corresponding author:
Deyana Ditto, Oral and Dental Health Services, Primary Health – Ministry of Health, Road 4025, Al Juffair 340, 12, Bahrain. Email: DDito@health.gov.bh
Received date: February 17, 2018; Accepted date: March 26, 2018; Published date: March 30, 2018

Background and objectives: Molar incisor hypomineralization (MIH) is a common developmental disturbance of the enamel involving the permanent incisors and first molars. There is no account of data regarding the prevalence of MIH in Bahrain, till date. The aim of the study was to ascertain the prevalence of MIH in seven–nine-year-old children attending government schools in Bahrain.
Methods: This cross-sectional descriptive survey consisted of 760 children aged seven–nine years, attending government schools located in the four governorates in Bahrain. Dental screenings were conducted and MIH was diagnosed according to the European Academy of Pediatric Dentistry, 2003 judgment criteria.
Results: The prevalence of MIH was 17.6%, which decreased with age. The highest prevalence rate was found in Muharraq and the odds of children diagnosed with severe MIH were more in the Southern Governorate. Demarcated opacity was the most common dental defect, which affected the molars and incisors. Significantly larger numbers of maxillary first permanent molars and incisors were diagnosed with MIH.
Conclusion: MIH was common in children’s permanent teeth, with some intra-country variation. A predilection for maxillary teeth being affected with MIH opacities was clearly revealed. There is a need for regular follow-ups with regard to the prevalence of MIH.
Keywords: Molar incisor hypomineralization, demarcated opacities, developmental dental defects, enamel defects, prevalence, proportion.
In recent years, in addition to dental caries, developmental defects of enamel called the molar incisor hypomineralization (MIH) have been recognized as increasing global issue. It is not a new phenomenon as it was first noted in Sweden in the late 1970s.1 The term MIH is used to describe hypomineralization of systemic origin affecting one or more first permanent molars (FPM) and is frequently associated with hypomineralized permanent incisors.2
Hypomineralization transpires due to the disturbance that occurs after the enamel layer has been secreted. It presents as translucency in enamel due to mineral deficiency and is known as opaque enamel. The opacity is sharply demarcated from normal enamel, and varies in color from white, cream, or yellow-brown. Therefore, these defects present with normal thickness of enamel at the time of eruption that rapidly disintegrate when exposed to the oral environment with unpleasant sequelae, such as premature enamel loss, sensitivity, and rapid caries development. The hypomineralization develops asymmetrically and either the FPMs or incisors or both are affected to differing extent in the same dentition.3
It is observed that by the age of nine, children affected with MIH generally undergo dental treatment for FPMs, nearly 10 times more often than healthy controls.4 Hence, once the permanent molars and incisors have fully erupted, there is a need for early detection of MIH in children in order to identify and treat it at an earlier stage, as these children are known to develop atypical caries requiring re-treatment.
The global prevalence of MIH ranges between 2.8%5 and 40.2%6 with the majority of the studies from the European countries; however, data is scarce in the regions of North America, Africa, and the Middle East.7, 8 Therefore, the purpose of the present study was to provide epidemiological data concerning the prevalence of MIH in representative samples of seven–nine-year-old children from the four governorates in Bahrain attending government schools.
The prevalence of MIH were determined as part of the first cross-sectional national oral health survey after obtaining ethical approval from the Ethical Committee, Ministry of Health, Kingdom of Bahrain. The study population comprised of 760 children aged between seven and nine years attending government schools in the four governorates of Bahrain, namely Muharraq, Capital, Northern, and Southern. The study was conducted during November 20–December 3, 2017. Children having at least one of the erupted index teeth, namely FPM and permanent incisors, as mentioned in the definition of MIH were included in the study.2 Children with changes in dental enamel, such as amelogenesis imperfecta, hypoplasia, diffuse opacities, white spot lesions, fluorosis, white cuspal, and marginal ridges were excluded.
The study sample was selected by stratified random procedure from the four governorates and schools. Simple random sampling was used to select the sample from each grade.9 Written consent was obtained from the school authorities and parents before the commencement of the study.
Prior to examinations, the two pediatric dentists were trained to diagnose and differentiate MIH using 15 photographs of varying presentations of the condition along with other dental defects. Then a group of 25 children aged between seven and nine years, who were not part of the study sample, were examined for calibration. The Cohen’s Kappa showed a very good agreement between the two investigators (Kappa=0.90, P<0.0001).
Children were examined in the classroom while lying down on a table using daylight supplemented with a portable penlight torch. Examinations were conducted individually using sterilized mouth mirrors, probe, gauze, and dental gloves. An oral examination was performed on wet teeth and visible plaque, if present, was removed by cleaning the teeth with gauze to help differentiate between opacities and white spot lesions.
Demarcated opacities (<1 mm) and diffused opacities were not recorded. Each index tooth was examined starting from upper right maxillary quadrant till the mandibular right quadrant. The labial/buccal, lingual/palatal, and occlusal/incisal surfaces were examined and scored according to the judgment criteria recommended by the European Academy of Pediatric Dentistry (EAPD), 2003.2
Descriptive statistics were calculated for both numerical and categorical variables. Chi square test was used to examine the relation between MIH and demographic factors. To determine the association in the sample group between MIH and other factors at tooth level Deneralized Estimating equation Analysis was used to account for correlated data. The explored factors were gender, governorate, side of the mouth (right/left) and arch (maxillary/mandibular). Odds ratio (OR) and corresponding 95% conï¬dence intervals (CI) were calculated. All the analyses were conducted using STATA 12.0, and P<0.05 was considered statistically significant.
Written consent was obtained from 767 of 800 parents/guardians indicating their permission to examine the children for MIH (response rate: 95.5%). In seven children aged seven years, all the four FPMs were unerupted, and hence were excluded from the analysis bringing the sample size to 760 children. The sample was divided into three age groups: seven-years-old (12.2%), eight-years old (38.4%), and nine-years-old (49.3%) with girls slightly more than boys (51.7% vs. 48.3%) The distribution of the study sample based on the area of residence were similar in all the four districts: Capital (24.7%), Muharraq (23.8%), South (24%), and Northern (27.5%).
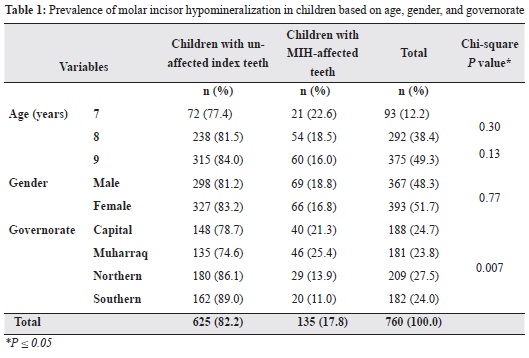
The prevalence rate of MIH was 17.8% (95% CI:15-20%). The only significant factor associated with MIH was the area of residence with Muharraq having the highest prevalence of MIH (25.4%) and the Southern Governorate having the lowest (11%; P value=0.007; Table 1). This was further supported by the Generalizing Estimating Equation analysis where the area of residence was the only significant factor after controlling for age and gender (Table 2). Compared to children living in the Muharraq Governorate, the odds of having MIH was 53% less in children living in the Northern Governorate (OR=0.47; P value=0.006) and 64% less in those living in the Southern Governorate (OR=0.35; P value=0.001). Although the odds of MIH was alsolower in children residing in the Capital Governorate compared to the Muharraq Governorate, this was not statistically significant (OR=0.78; P value=0.32).
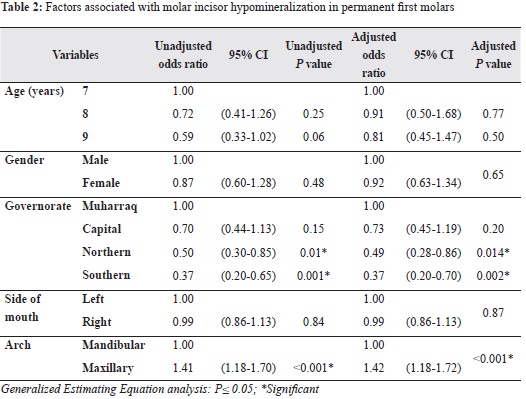
We reported a statistically highly significant difference between prevalence of MIH and dental arch. The risk of molars being affected by MIH in the maxillary arch was higher as compared to mandibular arch (OR=1.42; CI 1.18-1.72; P≤0.001). There was no significant difference between the prevalence of MIH and the side of jaw (Table 2).
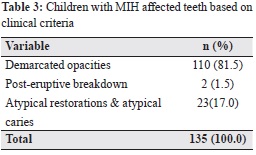
Demarcated opacities was the most common type of defect present and was observed in 110 children (81.5%). Atypical restorations and caries were recorded in 23 children (17%). The least common dental defect seen was post eruptive breakdown (PEB) observed in 2 children (1.5%). No missing index teeth due to MIH were identified (Table 3).
We reported the prevalence of MIH as 17.8%, which is in agreement with studies conducted in Finland (17%),10 Jordan (17.6%),11 and Sweden (18.4%)12 amongst seven–eight-year-old children. In contrast, Hong Kong (2.4%)5 recorded the least and Brazil (40.2%)6 the highest prevalence. The prevalence rates from different countries maybe incomparable owing to variations in judgment criteria, examination conditions, and sample selection. Our findings reveal MIH is moderately prevalent in Bahrain and can be considered as a global, rather than a regional problem.
Earlier studies have suggested the need for more research, especially in the Middle East, to understand the effect of geographical location on MIH as majority of the studies are clustered in Europe.13 Hence, we compared the prevalence range in Middle East regions as they are similar in culture and ethnicity.14 Bahrain displayed a higher prevalence rate as compared to Iran (12.7%),14 Istanbul (14.9%),15 Iraq (19%),16 and Saudi (8.6%),17 however, these findings need to be interpreted cautiously. The sample size was less for the Saudi study, and it reflected prevalence rate in both the Saudi and non-Saudi population with slightly more in the older children (8–12 years). In terms of Istanbul, although the age group examined was similar, MIH was diagnosed using different criteria, which might make it difficult to differentiate between demarcated and diffuse opacities. The study in Iran found that the difference in prevalence rates in the Middle East could be attributed to the difficulty in identifying the potentially affected unerupted index teeth. It was also concluded that future studies should use criteria that incorporate a specific eruption status scale in the clinical index of MIH.
We found that the area of residence was a major factor associated with children being affected with MIH. Therefore, we conclude that an intra-country variation in prevalence rate exists Bahrain, with the highest prevalence observed in Muharraq Governorate and the least in the Southern Governorate (25.4% and 11%, respectively). Similar intra-country variations in prevalence have been reported in Bosnia (9 cities),18 Netherlands (4 cities),19 Greece (3 cities),20 Jordan (3 cities),11 and Iran (4 zones).14 This intra-country variation may be considered as a peak phenomenon and maybe attributed to the population size. In terms of socioeconomic conditions, they were similar as the sample represented government schools only, and hence, our results cannot be extrapolated to the general population. Since we did not study the effect of environmental factors on MIH, our findings provide previously unavailable baseline data for Bahrain, and prospective studies should explore the sociodemographic effects on the population.
In the present study a significant difference was found between the number of affected teeth based on dental arch. The maxillary FPMs and incisors were affected to a larger extent than the mandibular teeth and was statistically highly significant. This is in agreement with studies involving samples from Bosnia18 and Greece.20 In contrast, Calderara et al. found no significant difference between the maxilla and mandible, with respect to MIH.21 This could be attributed to the chronological order of the human dentition in which maxillary teeth are generally ahead of mandibular teeth in development.22
Upon assessing the MIH-affected teeth based on clinical criteria, a wide variation of the lesion was noted. Demarcated opacities were the most common defect in both molars and incisors, which was similar to other studies.18, 21 PEB was the least observed defect with similar findings being reported by Preusser et al.23 MIH is dynamic in nature, which increases in severity with increase in age. The demarcated opacities are soft and porous in nature, which rapidly disintegrate along with loss of enamel.19, 23 The early identification of such children will allow monitoring of their FPMs so that remineralization and preventive measures can be instituted as soon as affected surfaces are accessible.
Some limitations were noted in this study. A larger sample size involving both the government and private schools would shed light on the true extent of MIH in the general population and help identify a gender difference, if present. The authors suggest further prospective longitudinal observational studies on larger populations to declare the exact environmental factors responsible for this type of enamel defect.
Based on this study’s results, the following conclusions can be made:
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.

Figure 1: Demarcated opacity in upper central and lateral incisors

Figure 2: Posteruptive enamel breakdown in FPMs

Figure 3: Atypical caries in upper central incisor