
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 1, Pages 14-18
https://doi.org/10.26715/jbms.p25_4Nazieha A. Al-Muzien,* Latifa S. Al-Sowielem**
*Qatif Primary Healthcare Centers, Eastern Province, Saudi Arabia
**Female Medical College, Dammam University, Saudi Arabia
Correspondence to: muzain_n@hotmail.com

Background: The prevalence of diabetes in Saudi Arabia ranks as one of the highest in the world. Many studies have found depression to be higher in diabetics than in the general population thus increasing costs and incidence of complications. To the best of our knowledge, no study has addressed the issue of depression in diabetics in Saudi Arabia.
Objectives: To assess the prevalence of depression and its associated factors in adult Saudi diabetics attending primary healthcare centers in the Qatif area.
Method: A cross-sectional study conducted in Qatif primary healthcare centers from January to February 2011. Nine centers were selected by stratified sampling. Systematic sampling of adult Saudi diabetics attending those centers was done and the selected patients were interviewed and asked to complete a two-page questionnaire, which included an Arabic version of PHQ9 depression questionnaire. Files of the interviewed patients were reviewed to assess the level of diabetes control.
Results: A total of 325 patients participated in the study. Prevalence of depression was found to be 14.5%. The prevalence of major depressive disorder was 6.2% and other depressive disorders were 8.3%. The presence of complications, co-morbidities and, in male patients, older age were found to be risk factors for depression in diabetics. The level of control was better in non-depressed patients while compliance with treatment had no relation with depression.
Conclusion: Depression is an important prevalent co-morbidity in diabetic patients. Screening for depressions an important part of comprehensive diabetic care. Further studies of depression in diabetics in Saudi Arabia are recommended.
Keywords: Qatif primary health care; depression; diabetes mellitus; PHQ-9
Saudi Arabia has witnessed massive socioeconomic development in the past 30 years. With increasing longevity and changes in lifestyle, there has been a consequent change in the pattern of diseases with a marked increase in illnesses related to non-communicable diseases, particularly cardiovascular diseases and diabetes.1, 2
Diabetes is an important global health problem. In 2010, the prevalence of diabetes was 284 million people constituting 6.4% of the world’s population.3 The prevalence of diabetes mellitus in Saudi Arabia is one of the highest in the world with the most recent study by Al-Nozha et al. (2004) showing a prevalence of 23.7%.4, 5
An increased prevalence of depression among diabetic patients compared with the general population is suggested by many studies.6, 7 However, the reported prevalence of depression in diabetics varies markedly due to variations in methodology.8 Patients with diabetes and depression are less likely to adhere to self-care, tending to miss their doses more frequently and subsequently having a higher incidence of complications, poor outcomes, and poor quality of life.8, 9, 10, 11
In many studies, the prevalence of depression was found to be higher in females, smokers, the obese, those with low income, type 2 diabetics on insulin and the unemployed.8,10, 12
To the best of our knowledge no study has addressed depression in diabetics in Saudi Arabia.
To assess the prevalence of depression and its associated factors in adult Saudi diabetics attending primary care centers in the Qatif area of the Eastern Province of Saudi Arabia.
The study was cross-sectional and conducted in Qatif primary healthcare centers from January to February 2011 to assess the prevalence of depression in adult Saudi diabetic attendees. Qatif city lies in the north-east of the Kingdom of Saudi Arabia and is 20 km north of Dammam, the capital of the Eastern Province. It has a population of 300,000. There are 26 primary healthcare centers in Qatif, and of the total number of patients attending those centers, 8,500 were diabetic patients.13
The data collection tool was a two-page questionnaire. The first page dealt with demographic and socioeconomic data beside medical history and details about diabetes (type, duration, type of treatment, complications and compliance to treatment). The second page was an Arabic version of patient health questionnaire 9 (PHQ9) obtained from Cardiometabolic risk management in primary care by Quality Improvement Team in Chronic Care (CCQI).15
The Patient Health Questionnaire PHQ9 is a nine-item questionnaire which helps to diagnose depression and assess its severity. It is based on the diagnostic criteria for major depressive disorder described in the Diagnostic and statistical manual, fourth edition (DSM-IV). Scores are categorized as minimal (1-4), mild (5-9), moderate (10-14), moderately severe (15-19) and severe depression (20-27).16
Sampling and data collection: nine out of 26 primary care centers in the Qatif area were selected by stratified sampling. Based on geographical location, centers were divided into central, east, west, north and south. In each area, random sampling was done to select the centers.
Every other Saudi adult (18 years or above) diabetic patient attending those centers was interviewed, after verbal consent was obtained, to complete the questionnaire. The interviews were conducted by the nurses covering the chronic disease clinics in those centers after they had been trained by the researcher. Files of the interviewed patients were reviewed to assess the level of diabetes control within the last year, using the latest HbA1C. If this was not available or unreliable as in the case of hemoglobinopathies, e.g. sickle cell disease and trait, the average of the latest three consecutive fasting blood sugar readings was used. HbA1C<7% or an average FBS <130mg/dl was considered good control; borderline control was HbA1C 7-8% or an average FBS 130-140mg/dl; and poor control was HbA1C>8% or an average FBS>140mg/dl.14
Data was analyzed using SPSS for Windows version 13.0 (SPSS Inc., Chicago, IL). Results were cross-tabulated to examine the relationships between the variables. Statistical analysis was performed using chi-square for test of association and Fisher’s exact test as appropriate. A P-value of less than 0.05 was considered significant in all statistical analyses.
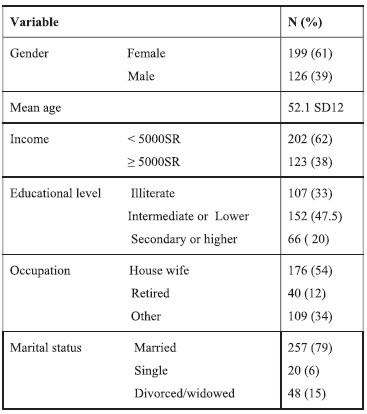
Three hundred thirty-seven patients were invited to participate. Three hundred twenty-five patients were interviewed yielding a response rate of 96.4%. Two-thirds of the sample were females, 199 (61.2%). The mean age was 52.1 years with a standard deviation of 12 years.
About two-thirds of the patients had a monthly income of less than 5,000 Saudi riyals. Many had an intermediate school certificate or lower, 152 (47.5%). About half the patients were housewives and a majority were married. (See Table 1 for details.)
Table 1. Demographic data
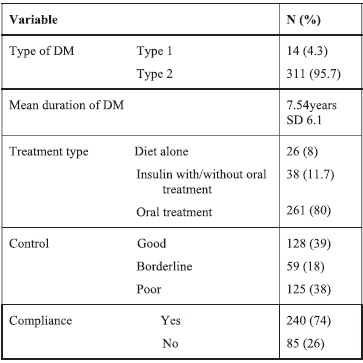
A majority of the patients were type 2 DM (Table 2). The mean duration of diabetes was 7.54 years with standard deviation of 6.12 years. Regarding the type of treatment used, insulin with or without other therapies was used in 38 patients (11.7 %), and diet alone was the treatment for 26 patients (8%). (Table 2)
Table 2. Diabetic disease information
Diabetic complications were present in about 17% of patients. The most common complication of diabetes reported was peripheral neuropathy 31(9.5 %), and the second most common was retinopathy 20 (6.2 %). The majority of patients had co-morbidities (85%), the most common being hypertension, 177 (54.5%), followed by dyslipidemia in 140 (43.1%). (See Table 3.)
Table 3. Frequency of co-morbidities
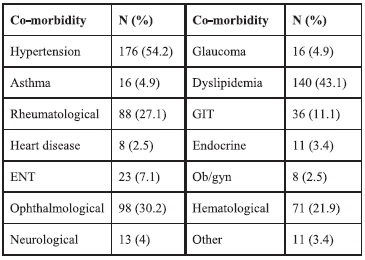
Of the co-morbidities, ophthalmological, ENT, rheumatological and neurological diseases were associated significantly with depression (P values of 0.022, 0.024, 0.001, and 0.005, respectively). With regard to the complications, only peripheral neuropathy was associated significantly with depression (P value <0 .001).
There was a significant association between the presence of co-morbidities and depression (P=0.028). (See Table 4.)
Table 4. Distribution of co-morbidities and complications in depressed vs. non-depressed patients
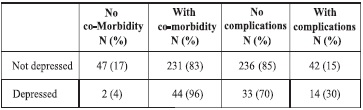
Chi-square of co-morbidity = 4.850 P=0.028
Chi-square of complication = 6.074 P=0.014
Diagnosed psychiatric illnesses were reported in 14 patients (4.3%), mostly depression in 8 patients. One patient had schizophrenia and 5 patients had other psychiatric illnesses including phobia, obsessive compulsive disorder and anxiety.
Most of the patients reported compliance to treatment (74.8%). The level of blood sugar control was good in 128 patients (39%), borderline in 59 patients (18.2%) and poor in 125 patients (38.5%).
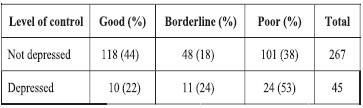
The level of blood sugar control was worse in depressed than non-depressed patients. (See Table 5.) No association between compliance and depression was found (P=0.108).
Table 5. Level of blood sugar control in depressed versus non-depressed patients
The prevalence of major depressive disorder was 6.2% (20 patients). Other depressive disorders were 8.3% (27 patients) and the overall prevalence of depression was 14.5% (47 patients). On the severity of depression, 25 patients had mild depression (PHQ9 score of =<15) while 22 had severe depression (PHQ9 score >15).
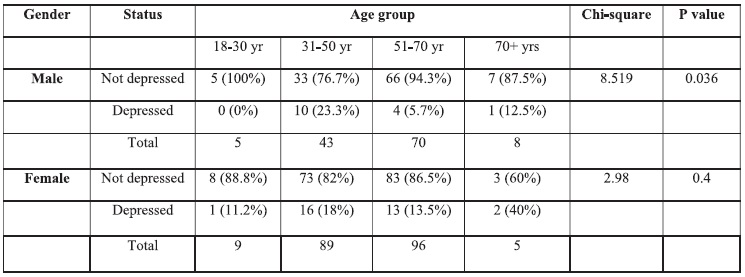
The duration of diabetes had no significant association with depression. Old age in male patients was associated with depression (P=0.036) while in females, it was not (P=0.4) (Table 6). No statistically significant association was found between work status, gender, educational level or income and depression. (See Table 6.). Furthermore, the type of treatment and duration of diabetes had no significant association with depression. Analysis of the severity of depression showed no correlation with any of the studied variables. (See Table 6.)
Table 6. Distribution of depression among gender and age groups
Screening diabetics for depression by means of standardized screening questionnaires could be an efficient way of identifying depression in those patients.17 The tool used for depression screening was PHQ9, which is well studied, and had been validated in Saudi Arabia in the study of Becker et al.18 Most of our patients were type 2 diabetics, which is in accord with the fact that 90% of diabetics worldwide and in Saudi Arabia are type 2.4
In this study, the prevalence of depression according to the PHQ9 questionnaire, was lower than that reported in the study by Becker et al. In that study, the prevalence of depression in primary care attendees at a university hospital was reported as 20%, but this might be due to different demographic characteristics.18 However, it is comparable to the results of Suliman et al. (12.5%) and the prevalence of mental illnesses in diabetic patients found in the Al-Kathami study (16% including somatization, anxiety and depression) but lower than that in the meta-analysis (31%) found in the self-administered questionnaire.6,19,20 The prevalence of major depression in our study is comparable to that reported in the USA (8.3%).12 The prevalence of diagnosed psychiatric illnesses was 4.3%, and previously diagnosed depression was only 2.4%, which reflects a large proportion of missed cases.
The presence of diabetic complications was associated with depression, which agrees with the findings of Suliman et al., and other studies.6, 20, 21 Of the complications, only peripheral neuropathy was significantly associated with depression. In our study, as expected, co-morbidities increased the risk of depression which supports the findings of Engum et al.22 Specific complications were significantly associated with depression in our study. These were ophthalmological, ENT, rheumatological and neurological diseases, possibly because besides impairing daily activity they are symptomatic unlike others like dyslipidemia. Unlike many studies we did not find any significant association between female gender and depression. This can be explained by the fact that the majority of our sample were females.6,13 Old age was the only significant factor for males. This agrees with the findings of Yekta et al. but contradicts some literature such as Katon.8, 20 There was no association between income and education with depression in our study in contrast to many others which show an increased risk of depression in poor and less educated diabetic patients.8, 21 An explanation could be the homogeneity of our sample regarding those factors.
Compliance, which was assessed by self-reporting, was not significantly associated with depression in contrast to what was expected. This was probably because patients had thetendency to hide their contribution to their poor control.8,23 The level of control was better in the non-depressed than the depressed, which accords with findings of many studies.6, 20 Severity of depression in our study was not associated with any of the studied factors probably due to the small number of depressed patients in our sample.
The constraints of time did not allow for a case control study, i.e. the comparison of the prevalence of depression in diabetic and non-diabetic patients. The study did not include important confounding factors such as obesity, smoking, physical inactivity and major life stressors like the loss of a spouse.
An assessment of complications and co-morbidities was done by self-reporting rather than from medical records, which may not be entirely reliable since many patients are followed in other clinics and charts available in primary care may not contain all the data.
I would like to express my sincere gratitude to Dr. Bader Al-Mustafa, Consultant, Family Medicine and clinical hypertension specialist, for his support and help. My thanks also go to all chronic disease nurses who participated in the study and to chronic care nursing supervisors, Farha Al-Marhoon and Manal Hijlis, for their assistance.