
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 1, Pages 46-48
https://doi.org/10.26715/jbms.p25_10Nada Al-Yousuf,*
*Department of Ophthalmology, Salmaniya Medical Complex, Kingdom of Bahrain
Correspondence to: nadaalyusuf@gmail.com

A case report of a 52-year-old Bahraini male who underwent pterygium surgery with amniotic membrane transplant without adjunctive therapy of mitomycin C or beta irradiation. Post operatively, he developed necrotizing scleritis at the site of pterygium surgery. He underwent conjunctival graft on the scleritis. One week post operatively, the conjunctival graft melted and the scleritis persisted. Subsequently, he had scleral patch graft on the scleral defect overlayed by a conjunctival autograft. His post-operative course was uneventful. This case shows that scleral melt can happen post pterygium surgery with amniotic membrane transplant. This complication is well documented following the use of adjunctive therapy such as mitomycin C or beta irradiation. It has also been reported following pterygium surgery with the bare scleral technique. To our knowledge this is the first reported case of necrotizing scleritis without adjunctive treatment and with amniotic membrane transplant. Ophthalmic surgeons should take this complication into consideration before any pterygium surgery.
Keywords: pterygium, necrotizing scleritis, scleral melt, scleral graft
Necrotizing scleritis is a localized area of severe scleral inflammation and melt. It is a serious and challenging problem which can be caused by a number of diseases. It can be associated with systemic autoimmune diseases without a history of ocular surgeries, and it can occur in an otherwise healthy individual following ocular surgery. It is a well-known complication after pterygium surgery if it is associated with the use of mitomycin C or with beta irradiation.1-5 Moreover, necrotizing scleritis has been reported following retinal surgery, cataract removal, squint surgery and trabeculectomy.1, 6 In such conditions it typically occurs as an intense scleritis at the site of limbal or scleral surgical incision. Furthermore, this complication has also been reported following pterygium surgery without amniotic or conjunctival graft, i.e. using the bare scleral technique.6 Post-operative scleritis can also be infective. Management is the biggest challenge. Different modalities of treatment have been described. Medical treatment includes systemic immunosuppression and systemic and topical nonsteroidal anti-inflammatory agents. Surgical treatment includes amniotic membrane transplant, tenonoplasty, buccal mucosal graft, scleral patch graft, tectonic lamellar corneal grafting and conjunctival autograft.8-10
We believe that scleral necrosis following pterygium excision with amniotic membrane transplant has not previously been reported in the literature.
ASM is a 52-year-old Bahraini male who had had pterygium surgeries done on both eyes in the past. The right eye was done 10 years ago and the left eye 15 years ago. The left eye was done by a colleague using the bare scleral technique. The right eye was done by us using a conjunctival autograft with pterygium excision. The right eye was asymptomatic with no recurrence. The patient subsequently developed recurrence of the pterygium in the left eye. He was managed conservatively for one year mainly with lubricants. The patient could not tolerate the pterygium which was interfering with his vision and comfort. His vision was 6/12 in the left eye and 6/6 in the right eye.
The patient underwent pterygium excision with amniotic membrane transplant without mitomycin or beta irradiation. He was prescribed topical antibiotics with corticosteroid combination as well as topical artificial tears. The patient did not use the antibiotic-steroids combination; he used lubricant only. On his one-week follow up, vision was found to have improved to 6/6. The eye was quiet, the amniotic membrane in place. He was asked to use his medication. A few days later, he developed severe pain. Examination revealed amniotic membrane disintegration at a localized part on the surgery site associated with a pinpoint scleral defect. The patient was scheduled for conjunctival autograft to cover the sclera at that point. Three days later, the scleral defect had increased in size to around 5 mm. (See Figure 1.) There was scleral melt with choroidal exposure. In addition to his medications, he was prescribed topical moxifloxacin hourly and was put on systemic prednisolone. Further, he was investigated for autoimmune disorders. The results came back negative. The following day he underwent conjunctival autograft. The surgery was uneventful. On his first day post op, vision was stable at 6/9, and the conjunctival graft was in place. Unfortunately, one week later, the conjunctival graft had disintegrated at that particular point. The scleral defect was revealed and the choroid was exposed. Fundus examination was normal throughout.

Figure 1. Necrotizing scleritis with scleral melt and minimal corneal melt post pterygium excision and amniotic membrane transplant
The patient then had scleral patch graft covering the scleral defect with conjunctival autograft.
Post operatively, the patient was prescribed topical moxifloxacin, a topical nonsteroidal anti-inflammatory, extensive lubrication, in addition to the systemic immunosuppression and brufen tablets. He was also given intravenous cefuroxime followed by tablets.
The patient recovered well, his post-operative follow-up visit showed vision 6/9 and the scleral graft and conjunctival graft were healing. (See Figure 2.)
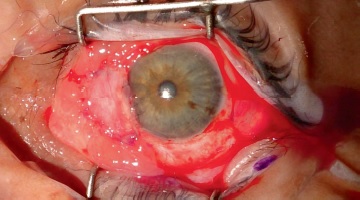
Figure 2. Post-operative photo after transplanting a scleral patch graft with overlying conjunctival autograft
This case shows that necrotizing scleritis is very challenging. The cause of the necrotizing scleritis was not obvious especially since the patient did not have any adjuvant treatments such as mitomycin C or beta irradiation. Also, the fact that amniotic membrane was transplanted at the surgical site makes it even more puzzling, because it is known that such cases had undergone either adjunctive therapy or the bare scleral technique. One possibility is that the scleritis could be infectious especially since the patient did not use his antibiotic-steroid drop combination on the first week following his surgery. Infectious scleritis has been reported in the medical literature following pterygium surgery.11, 12 Excessive cauterization during pterygium excision is another possibility and this has been documented in the literature.7
Pterygium surgery is one of the commonest surgeries in ophthalmic practice. Most ophthalmologists underestimate the complications associated with it. The case we present demonstrates that although this is a very simple extraocular procedure, it can be associated with devastating complications such as necrotizing scleritis.
Ophthalmologists should consider necrotizing scleritis as a possible complication following pterygium surgery, and this should be explained to the patient when obtaining consent for surgery. The use of a scleral patch with an overlying conjunctival autograft was shown to be effective in treating this disease.
1. Galanopoulos A, Snibson G, O’Day J. Necrotizing anterior scleritis after pterygium surgery. Aust N Z J Ophthalmol. 1994 Aug;22(3):167-73.
2. Tarr KH, Constable IJ. Late complications of pterygium treatment. Br J Ophthalmol. 1980 Jul;64(7):496-505.
3. MacKenzie FD, Hirst LW, Kynaston B, Bain C. Recurrence rate and complications after beta irradiation for pterygia. Ophthalmology. 1991 Dec;98(12):1776-80; discussion 1781.
4. Owoeye JF, Ayorinde OO. Surgically induced necrotising scleritis after pterygium excision. West Afr J Med. 2012 Mar-Apr;31(2):142-4.
5. Safianik B, Ben-Zion I, Garzozi HJ. Serious corneoscleral complications after pterygium excision with mitomycin C. Br J Ophthalmol. 2002 Mar;86(3):357-8.
6. O’Donoghue E, Lightman S, Tuft S, Watson P. Surgically induced necrotising sclerokeratitis (SINS)--precipitating factors and response to treatment. Br J Ophthalmol. 1992 Jan;76(1):17-21.
7. Alsagoff Z, Tan DT, Chee SP. Necrotising scleritis after bare sclera excision of pterygium. Br J Ophthalmol. 2000 Sep;84(9):1050-2.
8. Sangwan VS, jain V, Gupta P. Structural and functional outcome of scleral patch graft. Eye (Lond). 2007 Jul;21(7):930-5.
9. Tseng SCG, Casas VE. Cryopreserved amnion grafts and tenonplasty for scleral melt due to ischaemia. The Ocular Surface Research & Education Foundation. Available at:http://www.osref.org/media/documents/osref_guide_to_scleral_ischemia_and_melt.pdf
10. Ti SE, Tan DT. Tectonic corneal lamellar grafting for severe scleral melting after pterygium surgery. Ophthalmology. 2003 Jun;110(6):1126-36.
11. Pradhan ZS, Jacob P. Infectious scleritis: clinical spectrum and management outcomes in India. Indian J Ophthalmol. 2013 Oct;61(10):590-3.
12. Hodson KL, Galor A, Karp CL, Davis JL, Albini TA, Perez VL, et al. Epidemiology and visual outcomes in patients with infectious scleritis. Cornea. 2013 Apr;32(4):466-72.