
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 2, Pages 75-79
http://doi.org/10.26715/jbms.25_2_3Dalal Adnan Al-Hashimi,* Khaldoon Al-Roomi, ** Adel Salman Al-Sayyad, ***
*Consultant Family Physician, Ministry of Health, Manama, Kingdom of Bahrain
**Dean, College of Medicine & Medical Sciences, Arabian Gulf University, Kingdom of Bahrain
***Disease Control Section, Public Health Directorate, Ministry of Health, Manama, Kingdom of Bahrain
Correspondence to: dhashimi1@health.gov.bh

Background: Poor compliance by physicians with communicable diseases reporting is a worldwide phenomenon. In Bahrain, there are limited data regarding thoroughness and completeness of the current communicable diseases reporting system.
Objective: To identify reasons for noncompliance with reporting of notifiable communicable diseases by primary health care physicians practicing in the Ministry of Health (MoH) primary health care centers.
Methods: This is a cross-sectional study. Two hundred and forty-one self-administered questionnaires were distributed to all primary health care physicians practicing in all primary care health centers of the Ministry of Health. The questionnaires included items regarding socio-demographic and practice-related characteristics, self-reported practice related to communicable diseases reporting and reasons for noncompliance with reporting requirements.
Results: The response rate was 93%; the mean age of the respondents was 43 ±8.36 years. The period of experience in clinical practice ranged from 1 to 35 years with a mean of 12.84 ± 7.86 years. Lack of feedback on notified cases, forgot to notify, and not sure of diagnosis were cited by more than half of the physicians as reasons for noncompliance with communicable diseases reporting.
Conclusion: The findings suggest that there are several reasons for noncompliance with reporting requirements. Revising the current notification procedure to resolve some of the reasons is vital to enhance communicable diseases reporting in Bahrain.
Keywords: Bahrain; communicable diseases; notification; reporting; reasons
Epidemiological surveillance has been defined as “the ongoing and systematic collection, analysis and interpretation of health data in the process of describing and monitoring a health event”1. The important role of surveillance in reporting, monitoring, and responding to infectious diseases has been stressed by the World Health Organization (WHO).
Surveillance data are useful in many ways, including assurance of provision of appropriate medical therapy, detection of common source outbreaks, and providing the basis for planning and implementing prevention and control programs. Policy makers need such data in order to determine public health priorities for public health programs and to evaluate the success or failure of prevention and control programs2.
The literature suggests that the occurrence of notifiable infectious diseases is seriously underestimated due to underreporting. This negatively impacts on the effectiveness of the notification process as a real-time surveillance tool and an early warning system for outbreaks. In many countries, under-reporting is a common problem of the communicable diseases notification systems3-11. Arab countries are not an exception12, 13. Therefore, researchers in different parts of the world have investigated reasons for noncompliance with communicable diseases notification (CDN).
The factors that contribute to under-reporting are diverse. Hence, some authors have pointed to lack of awareness regarding notifiable diseases14-16, or physicians’ attitude towards the notification system as responsible factors17, 18. However, it is not only knowledge and attitude that are directly translated into practice, other external factors also influence this process such as lack of time, concern about patient confidentiality, complexity of the reporting procedures, poor accessibility to notification materials, lack of motivation secondary to lack of feedback, and an assumption that somebody else will report. e.g., lab technicians and other specialists19-26.
The system of communicable diseases reporting in Bahrain was established in 1955 and the surveillance system was strengthened in 1971, whereby registers for selected communicable diseases are maintained27. Public health officials rely on health providers, laboratories and other public health personnel to notify of the occurrence of infectious diseases to the Communicable Diseases Unit (CDU) of the Ministry of Health. According to the current notification regulation in MoH health centers all practicing primary health care physicians are required to notify of relevant communicable diseases via stamping patients’ prescriptions with the communicable diseases stamp, subsequently sending the patient to nursing staff who should fill in the form, to be returned within a week via hand, post or fax. For some diseases an immediate telephone notification is mandated, followed by written notification within 24 hours.
In Bahrain, there are limited data regarding thoroughness and completeness of the current communicable diseases notification system. However, observations by public health officials in the MoH strongly suggest that a problem does exist in Bahrain. The number of notified cases by physicians was perceived not to reflect the actual occurrence of infectious diseases when compared to that reported by the Public Health Laboratory. Thus, a need exists to explore the reasons for under-reporting.
The aim of this study is to identify reasons for noncompliance with optimal notification requirements by primary health care physicians practicing in MoH primary health care centers in Bahrain.
This study is a cross-sectional, descriptive study involving all physicians practicing in Ministry of Health primary health care centers (PHCC) in Bahrain including both family physicians and general practitioners. At the time of conducting the study there were 271 primary health care physicians (PHCP) practicing in twenty-two PHCC that are distributed throughout Bahrain. Primary health care physicians who were involved in administrative work only and have no access to clinical practice were excluded. The sample size was 261 physicians as ten physicians were involved in administrative work only and were not running regular clinics in the health centers.
The study instrument was a self-administered, structured questionnaire which was partially developed and modified by the researchers based on a literature review of studies conducted to investigate reasons for under-reporting of notifiable diseases17, 18, 25, 28. The questionnaire included the following items: socio-demographic and practicerelated characteristics (age, gender, specialization, years of experience), physicians’ self-reported practice (the number of cases that the participants diagnosed within the past three months and the number of cases which were notified from the diagnosed cases), and reasons for noncompliance with reporting requirements which were identified by using a predetermined checklist. The checklist contained 12 items, the participants were asked to mark either “Yes” or “No” for each item (Table 3).
The questionnaire was piloted in order to check the clarity of the questions and reliability of the questionnaire using a sample of 20 PHCPs. Accordingly, minor changes were made based on feedback from the participants. The participants in the pilot study were not included in the main study. Content validity has been assessed by public health specialists and the academic committee to evaluate the items’ readability, suitability, and to evaluate the relationship of each item to the whole scale. The internal consistency reliability of the questionnaire has been assessed using Cronbach’s alpha which was 0.74. The participation in the study was voluntary and confidentiality was assured through number coding of questionnaires to protect privacy.
The self-administered questionnaires were distributed to all physicians practicing in government health centers at the time of conducting the study along with a covering letter addressed to the participants briefing them on the purpose of the study and assuring confidentiality. The questionnaires were collected from the health centers heads of council within two weeks.
The data were analyzed using SPSS version 15 and relevant descriptive analyses were performed for all items. Variables were presented either as frequencies for categorical variables or means with standard deviation for quantitative variables. The Pearson’s Chi-square test was used to compare proportions. Statistical significance was set at P-value <0.05.
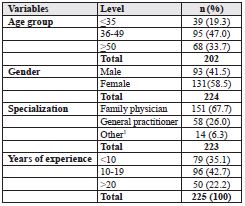
A total of two hundred and forty-one questionnaires were distributed to all eligible primary health care physicians practicing in MoH health centers in Bahrain (20 physicians who were involved in the pilot study were excluded). 225 questionnaires were returned yielding an overall response rate of 93%. The mean age of the respondents was 43.00 ±8.36 years with a median age of 43 years. The period of experience in clinical practice ranged from 1 to 35 years with a mean of 12.84 ±7.86 years and a median of 12.0 years. Female physicians constituted more than half of the sample (58.5%). About two-thirds of the sample had family medicine qualifications (67.7%). (See Table 1)
Table 1. Participants’ socio-demographic and practicerelated characteristics
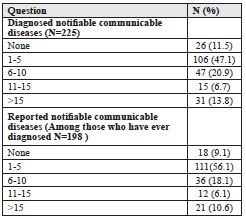
With regards to physicians’ reported CDN practice, 198 (88%) physicians stated that they have diagnosed notifiable communicable diseases within the last three months. One hundred and eighty physicians (90%) stated that they had ever reported a notifiable communicable disease, whereas 18 (10%) stated that they had never reported any notifiable communicable disease within the last three months even when diagnosed. Assuming the average number of cases, the total number of diagnosed notifiable conditions was found to be 1,403, and the total number of notified cases was 1,134. This indicates that 80% of the diagnosed communicable conditions were notified while 20 % were not (see Table2).
Table 2. Diagnosis and reporting experience of notifiable communicable diseases among the primary health care physicians within the last three months
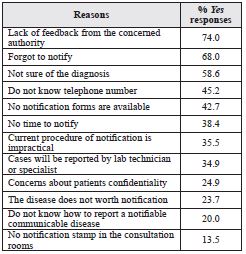
As is shown in Table 3, lack of feedback from the Public Health Directorate was the most commonly cited reason for noncompliance with communicable diseases notification followed by physicians’ forgetfulness to notify. Furthermore, over half of the PHCPs cited uncertainty of diagnosis as a reason for under-reporting (58.6%). Unfamiliarity with the CDU telephone number and unavailability of the notification forms were considered as reasons by 45.2% and 42.7% respectively. More than onethird of the physicians (38.4%) considered lack of time, impracticality of the current notification procedure (35.5%) and assumption that reporting will be done by other staff (34.9%) as a cause for not notifying. One-fifth of the participating physicians (20%) cited “do not know how to notify a notifiable communicable disease” as a reason for not reporting.
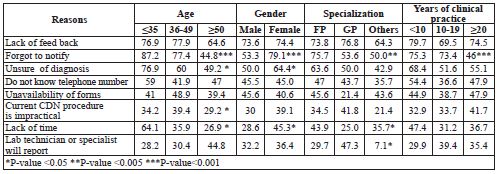
Ranking of reasons for under-reporting of communicable diseases didn’t vary much when the analysis was repeated according to age, gender, specialty and years of clinical practice. In all categories lack of feedback from the Public Health Directorate, forgot to notify and not sure of the diagnosis were in the top of the list for all mentioned categories.
Table 3. Percentage of primary care physicians marking “Yes” on reasons for noncompliance with communicable diseases notification requirements (N=225)
The possible relationship between the socio-demographic characteristics of the participants and their responses to the questionnaire was investigated. It was found that the female physicians were more likely to consider forgetfulness to notify (79.1%), lack of time (45.3%) and uncertainty of diagnosis (64.4%) as reasons for noncompliance compared to male physicians, 53.3%, 28.6% and 50.0% respectively. The differences in the proportions were statistically significant (Table 4).
Likewise, physicians who were less than 35 years old were more likely to consider these factors as reasons for not reporting than the older age groups namely: forgot to notify (p<0.001), lack of time (P=0.007), and uncertainty of the diagnosis (P=0.024) (Table 4). Family physicians were more likely to cite forgot to notify (P=0.003), and lack of time (P=0.045) as reasons for not notifying than the general practitioners or other specialty colleagues (Table 4).
Table 4. Reasons for noncompliance with communicable diseases notification requirements by primary care physicians’ socio-demographic characteristics (N=225) (P value based on chi -square)
The most common reasons for failure to notify communicable diseases in this study were lack of motivation secondary to poor feedback from the concerned authorities, forgot to notify, not sure of diagnosis, unawareness of telephone contact number to notify, and poor accessibility of the notification forms. These reasons are similar to those found in other studies19-21, 25, 26, 29.
This study revealed that almost three-quarters of the physicians (74%) considered lack of feedback from the concerned authorities as a reason for not complying with CDN. This figure is significantly higher than that found in other similar studies21, 30. Lack of feedback from the concerned authorities is a well-recognized barrier to CDN in most of the Mediterranean region, as this mechanism is among the weakest points of the surveillance system in the region31. There is usually no way of showing health workers the value of their vital contribution to the system and, hence, they lose interest in surveillance activity13, 20, 21, 24, 30, 31. Therefore, several studies have been conducted to find ways to improve notification practice of communicable diseases. All suggested that feedback to physicians showing them that preventive action is taken as a result of their notification can be an effective way to improve notification practices 23, 30, 32, 33.
In the present study forgot to notify was cited by 68% of the participating physicians as a reason for not notifying communicable diseases. This figure is consistent with that found in Sri Lanka18. This finding could be explained by short consultation times in the primary health care center, i.e. 7.5 minutes per patient. Lack of time has been identified as a reason for under-reporting of communicable diseases in many papers16, 18, 19, 22, 26, 29. In this study lack of time was identified by 38.4% of the physicians as a reason for not notifying. The existing CDN procedure regulations are intended to reduce physicians’ workload through assigning the CDN form-filling responsibility to nurses, a measure which has been found to increase physicians’ compliance to notification in several studies22. It seems that practicing primary care physicians still consider this duty as time consuming. Therefore, this negative attitude needs to be modified through improving physicians’ knowledge regarding the role of CDN in communicable diseases control and constantly reminding the physicians about the notifiable diseases surveillance system.
Not sure of the diagnosis was cited as a cause for not complying with communicable diseases notification by more than half of the physicians (58.6%). This result is in agreement with that of the Lee and Meng study which was conducted in Korea34. The results of this study revealed that uncertainty of diagnosis was a major reason for not notifying. This finding implies that lack of knowledge regarding notification requirements is a contributing factor for under-reporting. Cases reported by laboratory technicians or a specialist were cited as a reason by 34.9 % of PHCPs. This finding is in agreement with results of other studies in other parts of the world including USA28, Portugal26, and Malta30. Obviously, this finding reveals the reliance of the primary care physicians on hospital physicians and/or laboratory technicians to notify their suspected cases. Although laboratories can provide an important source of communicable diseases surveillance, it is not a substitute for physician notification, since there are a number of notifiable diseases, such as meningococcal infections, for which timelines of notification is an important factor, and waiting for a test result is not practical. Therefore, the duty to notify of communicable diseases regardless of hospital referral or laboratory confirmation is one area where clarification of notification requirements by the public health officials is needed.
Unavailability of CDN notification forms was cited as a reason for noncompliance with CDN by more than 40% of the participants in the present study. This reason has been pointed out by some researchers19, 25 as a major barrier to CDN suggesting that not only human factors are responsible for non-compliance with CDN, the notification system itself could be a main obstacle to CDN. Given the fact that the nurse is the responsible staff for filling the notification forms in the health centers, the responses of the physicians in the present study uncover the lack of knowledge concerning the current CDN requirement in primary health care centers.
In the present study, more than one-third of the physicians (35.5%) cited the impracticality of the current communicable diseases notification procedure as a cause for noncompliance with CDN requirements. This finding is comparable to that of Tan et al.23 and Abdool Karim and Dilraj19 , and it implies that the current CDN procedure in the MoH primary health care centers should be evaluated and revised in order to guarantee the utmost compliance with communicable diseases notification requirements in the Kingdom of Bahrain.
The study results identified that there are several reasons for noncompliance with communicable diseases notification requirements. With the emergence of new communicable disease pandemics, it is crucial that the Public Health Directorate at the MoH discuss these reasons with the frontline health workers, and involve them in devising solutions in order to improve their compliance.