
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 2, Pages 93-97
http://doi.org/10.26715/jbms.25_2_6Khalid A. Beerdawood*, Faiez D. Alhmoud**, Atef A. Al Namoura***, Abdel Hadi S. Al Briezat****
*Consultant General Surgeon, Ministry of Health, Amman, Jordan
**Consultant General Surgeon, Head of Surgical Department, Al Bashir Teaching Hospital, Ministry of Health, Amman, Jordan
***Specialist General Surgeon, Al Bashir Teaching Hospital, Ministry of Health, Amman, Jordan
****Consultant General Surgeon, Head of Surgical Specialty, Al Bashir Teaching Hospital, Ministry of Health, Amman, Jordan
Correspondence to: khaleddwd_1968@yahoo.com

Background: Mechanical bowel preparation was regarded for a long time as a vital prerequisite for successful colorectal surgery; this is now being questioned. The distressful effect of bowel preparation, alongside the safety of primary colorectal anastomosis in emergency cases, has led to a considerable change in the surgical protocol, making primary repair and anastomosis after colon resection safer without bowel preparation, and the role of colostomy has changed from mandatory to optional.
Aim: To assess whether colorectal surgery can be performed safely without mechanical bowel preparation or colostomy.
Method: A series of 130 patients, who underwent elective and emergency colorectal surgery, were followed prospectively over a three-year period in Al Bashir Teaching Hospital, Amman, Jordan. The patients were randomized into two groups. In one group (preparation group) 66 elective patients were selected from the outpatient department; the bowel was prepared using Fortran’s solution. In the second group (non-preparation group), 64 patients were selected from the emergency and outpatient departments, no bowel preparation was used. Colostomy was omitted in both groups. The main outcomes regarding operative time, hospital stay, rate of postoperative wound infection, anastomotic leak and intra-abdominal abscess were compared between the two groups.
Results: Malignancy was the most prevalent pathology in both the preparation and non-preparation groups, 75.7% and 62.5% respectively, while benign diseases were present in up to 24.2% of the preparation group and in 1.5% of the non-preparation group. Anastomosis was ileo-colic in 33.3% and 37.5%, colo-colic or colo-rectal in 66.6% and 62.5% of the preparation and non-preparation groups respectively. There was no significant statistical difference in the overall postoperative complication rates between the two groups, 16.6% in the preparation group and 14% in the non-preparation group. Postoperative wound infection, wound dehiscence, intra-abdominal abscess and anastomotic leak occurred in 9.09%, 1.5%, 1.5% and 4.5% in the preparation group, as compared to 7.8%, 3.1%, 0% and 3.1% in the non-preparation group respectively. The mortality rate was nil in both groups.
Conclusion: Resection of colorectal pathology followed by primary anastomosis, without stoma, can be performed safely with the omission of preoperative mechanical bowel preparation.
Keywords: colorectal surgery; primary anastomosis; mechanical bowel preparation; anastomotic leak; stoma
In the past, the mortality rate following colorectal surgery approached 20%, which was usually as a result of anastomotic leak and sepsis.1-6 It was generally believed that colon fecal load had an adverse effect on healing of the suture line.7, 8 This hampered primary colon anastomosis unless preoperative mechanical bowel preparation and antibiotic prophylaxis has been undertaken in the presence of healthy bowel, sufficient blood supply, tension-free and water-tight suture placement.9, 10 Nichols and Condon11 in 1971 demonstrated that mechanical removal of fecal load in patients undergoing colorectal surgery dramatically decreases postoperative morbidity and mortality rates.
The concept of mechanical bowel preparation would appear to have many advantages: it decreases contamination of the peritoneum and wound by reducing the intraluminal bacterial load, which in turn decreases the incidence of anastomotic dehiscence and makes bowel handling during surgery easier.12, 13 This current practice of mechanical bowel preparation before colorectal surgery is now being questioned. Its benefit has never been unequivocally proven in previous studies, and, on the contrary, some studies have shown that mechanical bowel preparation increases the incidence of wound infections and anastomotic leaks.14, 15
The distressful and unpleasant effects of mechanical bowel preparation, with enhanced bacterial translocation and adverse effects on anastomotic healing, has resulted in a change of the paradigm in respect to the need for bowel cleansing before colorectal surgery.16-18
Until recently emergency surgery for colon obstruction and injuries was managed by a staged procedure, the damaged colon either exteriorized, or repaired with protective colostomy.19 Primary anastomosis was contraindicated in such circumstances for fear of sepsis and suture line leaks. The psychological and physical impact of stoma on patients, with the added expense of stoma care and a second surgery for closure, beside a paucity of published studies confirming the efficacy of diverting colostomy in preventing anastomotic leak, questions the surgical principles in managing emergency colon surgery. This had led to a considerable change in surgical protocols around the world, and recent published studies have shown that primary repair and anastomosis after colon resection is safe, and the role of colostomy, instead of being mandatory, has become optional.20-22
A series of 130 patients were studied prospectively in Al Bashir Teaching Hospital, Amman, Jordan, over a 3-year period (2009-2012). All had undergone colorectal resection, or repair, with primary anastomosis for different pathologies. Patients were randomized into two groups and managed by two surgical teams. In one group (preparation group), 66 elective patients with presentations suggestive of colorectal pathology were selected from the outpatient department. Radiologic, endoscopic and biopsy studies confirmed colorectal disease mandating operative intervention. All patients were admitted on the day before surgery and received mechanical bowel preparation with four sachets of Fortran’s solution 12 hours before surgery, a soft diet was allowed until evening time. Resection of colorectal pathology was followed by primary anastomosis without stoma. In the second group (non-preparation group) 64 patients were selected from the emergency and outpatient departments with clinical diagnosis of intestinal obstruction, abdominal trauma, or signs and symptoms of colon pathology. Emergency and planned colorectal resections with primary anastomosis were undertaken, neither colostomy nor mechanical bowel preparation was used. Intravenous antibiotics were given to all patients in both groups at induction of anesthesia and continued for three doses postoperatively. Prolonged courses of intravenous antibiotics were given for any post-operative infections.
Laparotomies were carried out through midline approach; colorectal pathologies were dealt with accordingly by suture repair, or divided between non-crushing clamps. Bowel ends were cleaned with saline impregnated gauze, anastomosis was completed by a hand sewn single, mucosalinverting, layer of 3/0 vicryl suture, or staplers. Integrity of anastomosis was checked by increasing intraluminal pressure manually, looking for any gas or fecal leak. Drains or stoma were not used.
Data relative to patients’ demographics, diagnosis and operative procedure were recorded. The main outcomes regarding operative time, hospital stay, rate of postoperative wound infection, anastomotic leak and intraabdominal abscess were compared between the two groups.
Wound infection was defined as discharge of pus, wound erythema or a positive culture. Anastomotic leak was defined as a fecal discharge from the abdominal wound, vagina, intraperitoneal abscess or peritonitis.
Data from two groups were compared using chi square test, with a P-value of 0.05% considered to be statistically significant.
Table I. Demographic and clinical data
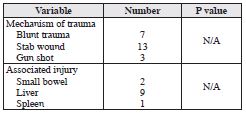
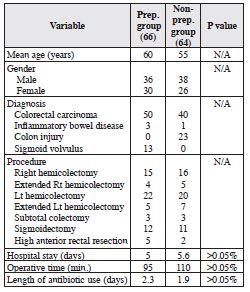 There were more male than female patients in both preparation (54.5% versus 45.4%) and non-preparation (59.3% versus 40.6%) groups respectively. The average hospital stay was similar for patients in the two groups. Histopathology of the resected specimens showed malignancy as the most prevalent pathology in both preparation and non-preparation groups, 75.7% and 62.5% respectively, while benign diseases were present in up to 24.2% of the preparation group and in 1.5% of the nonpreparation group (see Table I). Surgery for colon injuries constituted about 35.9 % of cases of the non-preparation group, with stab wounds comprising the major indication for laparotomy in 56.5% of them. All associated injuries were evaluated and treated accordingly, the liver being the organ injured most commonly (see Table II). All procedures were undertaken by consultant surgeons, with colo-colic or colorectal anastomosis representing about 66.6% and 62.5% of the preparation and non-preparation cases respectively, the majority being performed by hand-suturing technique. The anastomosis was ileo-colic in 33.3% and 37.5% of preparation and non-preparation groups respectively.
There were more male than female patients in both preparation (54.5% versus 45.4%) and non-preparation (59.3% versus 40.6%) groups respectively. The average hospital stay was similar for patients in the two groups. Histopathology of the resected specimens showed malignancy as the most prevalent pathology in both preparation and non-preparation groups, 75.7% and 62.5% respectively, while benign diseases were present in up to 24.2% of the preparation group and in 1.5% of the nonpreparation group (see Table I). Surgery for colon injuries constituted about 35.9 % of cases of the non-preparation group, with stab wounds comprising the major indication for laparotomy in 56.5% of them. All associated injuries were evaluated and treated accordingly, the liver being the organ injured most commonly (see Table II). All procedures were undertaken by consultant surgeons, with colo-colic or colorectal anastomosis representing about 66.6% and 62.5% of the preparation and non-preparation cases respectively, the majority being performed by hand-suturing technique. The anastomosis was ileo-colic in 33.3% and 37.5% of preparation and non-preparation groups respectively.
Table II. Mechanism of trauma and clinical data
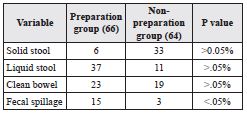
 Solid stool in the colon was the predominant finding in the non-preparation group, 51.5%, while liquid stool was present in up to 56% in the colon of the preparation group. Intraoperative spillage of fecal content was significantly higher in the preparation group, 22.7%, than the nonpreparation group, 4.6%, P value <0.05% (see Table III).
Solid stool in the colon was the predominant finding in the non-preparation group, 51.5%, while liquid stool was present in up to 56% in the colon of the preparation group. Intraoperative spillage of fecal content was significantly higher in the preparation group, 22.7%, than the nonpreparation group, 4.6%, P value <0.05% (see Table III).
Table III. Intraoperative assessment of bowel content and fecal spillage
There was no significant statistical difference in the overall postoperative complication rates between the two groups, 16.6% in the preparation group and 14% in the non-preparation group. Postoperative wound infection was slightly higher in patients of the preparation group, 9.09%, as compared to patients in the non-preparation group, 7.8%. The incidence of anastomotic leak and wound dehiscence in the preparation group was 4.5% and 1.5%, while patients of the non-preparation group showed an incidence of 3.1% and 3.1% respectively. One patient in the non-preparation group required reoperation for closure of a dehiscent wound (see Table IV). An intra-abdominal abscess occurred in only one patient in the preparation group, proving to be a minor anastomotic leak which closed spontaneously. The mortality rate was nil in both groups.
Table IV. Postoperative complications
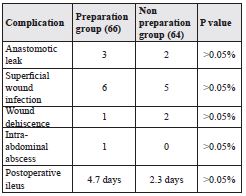
The use of mechanical bowel preparation before colorectal surgery has been surgical dogma for some considerable time, because it was considered to reduce the rate of infectious complications.23 But a number of prospective randomized studies have failed to show any significant difference in the rate of anastomotic leak and wound infection in patients with or without bowel preparation.24, 25 Burke et al. in 1994 published a study on 186 patients undergoing left colorectal resection, some received bowel preparation, others did not. These investigators failed to find a significant difference in the percentage of anastomotic leak and wound infection between the two groups, 3.7% and 4.9% for the preparation group, versus 4.6% and 3.4% in the non-preparation group respectively.26 Other studies have shown a significant increase in the incidence of anastomotic leak and wound infection in patients receiving mechanical bowel preparation (10% and 24% respectively) as compared to patients without preparation (5% and 12% respectively).27 In our study the rate of anastomotic leak and wound infection was lower in patients not receiving mechanical bowel preparation (3.1% and 7.8% respectively) as compared to patients receiving bowel preparation (4.5% and 9% respectively), but the difference was not statistically significant. Changing the physical characteristics of feces from solid to liquid, induced by cathartics during bowel preparation, makes it less controllable with more spillage of fecal material from the fresh anastomotic line.28, 29 Liquid stools were found in 56% of patients of the preparation group in our study, and control of intraoperative fecal spillage was significantly difficult in 22.7% of cases of the preparation group as compared to 4.6% of cases of the non-preparation group, P value <0.05%. This may explain the higher incidence of wound infection in patients in the preparation group (see Table IV).
Mechanical bowel preparation is not without its disadvantages; it causes fluid and electrolyte disturbance, abdominal pain and bloating. Furthermore bowel preparation may deplete colonic fatty acid and disturb the colon mucosal barrier thereby enhancing bacterial translocation, leading to an increased incidence of anastomotic leak, wound infection and other perioperative complications.30, 31
The safe results of primary anastomosis in the management of an unprepared colon in emergency surgery, obstruction or trauma, questions the necessity of mechanical bowel preparation.32-34 In the current series of 23 patients with various kinds of abdominal trauma, all were managed soon after hospital admission by primary repair or anastomosis without stoma. Two cases of gunshot injuries were managed by resection and primary anastomosis of the left colon and small bowel, one of them developing low output fecal fistula, treated conservatively, and the other one developing abdominal dehiscence that required reoperation for wound closure. However, 12 cases of colon obstruction treated with urgent resection and primary anastomosis without stoma underwent a smooth postoperative period except for one case that developed deep wound infection, which proved to be a minor anastomotic leak.
Frequently, when surgeons decide to create a defunctioning stoma this is based on a belief that a difficult anastomosis might leak. When the real indications of colostomy are not present, i.e. feculent peritonitis, low rectal excision, shock, poor nutritional status and neoadjuvent radiochemotherapy, stoma should be avoided, as it has not been shown to prevent anastomotic leak.35, 36 However, animal studies have shown that colostomy might impair anastomotic healing. Omission of stoma in our study showed no increase in the incidence of anastomotic leak and wound infection when compared with other studies where a stoma is created to protect an anastomosis. 37-39
Current data from randomized controlled studies showed no benefit of routine drainage after uncomplicated colorectal surgery, and on the contrary it might increase the incidence of anastomotic leak and wound infection.40, 41
Whether a handsewn or a stapler device is used for secure anastomosis, many controlled trials have shown no significant difference in terms of postoperative complication rate.42, 43
We report that resection of colorectal pathology followed by primary anastomosis, without stoma, can be performed safely with the omission of preoperative mechanical bowel preparation. Stoma should be strongly recommended when the patient has: shock, gross fecal peritonitis, low rectal anastomosis, multiple injuries and associated comorbidities. Antibiotic prophylaxis is recommended at induction of anesthesia and for two doses postoperatively, prolonged courses may be required in cases of infectious complications. Handsewn or stapled anastomosis produce the same results with respect to anastomotic leak.