
Journal of the Bahrain Medical Society
Year 2014, Volume 25, Issue 2, Pages 111-112
http://doi.org/10.26715/jbms.25_2_12Basem Abbas Al Ubaidi*
*Consultant Family Physician, North Muharraq Health Centre, Kingdom of Bahrain
Correspondence to: bahmed1@health.gov.bh

A sixty-seven-year-old female patient presented with symptomatic hypercalcemia as the first manifestation of primary hyperparathyroidism due to parathyroid adenoma. Initially the chronic hypercalcemia was investigated and then subsequent parathyroidectomy was done. She is doing very well six months following the surgery and the hypercalcemia has resolved completely.
Asymptomatic hypercalcaemia due to primary hyperparathyroidism is a common condition in primary care1. Most commonly primary hyperparathyroidism is caused by a solitary parathyroid adenoma (80%), and less frequently multi-glandular adenoma, parathyroid hyperplasia or carcinoma2. Patients rarely present with symptomatic hypercalcemia (mnemonic “stones,” “bones,” “abdominal moans,” and “psychic groans”) whereas usually patients remain asymptomatic and the condition is discovered during routine checkup investigations3. The disorder can occur at any age, yet is more common in the middle age group (≥50 years). The ratio of such cases is equivalent to 1:1000 in males, whereas it is 3:1000 in the female population4.
Hypercalcemia may be categorized based on total serum and ionized calcium levels (see Figure 1).
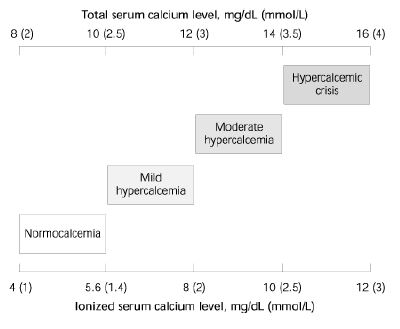 Figure 1: Spectrum of hypercalcemia5
Figure 1: Spectrum of hypercalcemia5
The aim of this report is to highlight hypercalcemia presentation in primary care.The aim of this report is to highlight hypercalcemia presentation in primary care.
A sixty-seven-year-old female presented to the noninfectious chronic disease clinic in primary care (NCD) with controlled diabetes mellitus Type 2, hypertension, and hyperlipidemia. There was a history of symptomatic hypercalcemia (fatigue, bone pain, mood disturbances, and cognitive impairment) which had gradually increased over the last 2 years. Initially, she was diagnosed with drug-induced hypercalcemia due to iatrogenic use of calcium which was prescribed by another physician for osteopenia 6 months earlier. The patient stopped calcium tablets but the hypercalcemia remained high. There was a history of nephrolithiasis four years previously. There was no significant family history. The patient looked healthy and her vital signs were normal. Cardiovascular, chest and abdominal examinations were unremarkable. No abnormality was detected in the musculoskeletal system. Investigations showed WBCs 14,000, lipase 1,395 u/l, serum calcium 3.5 mmol/L (2.21-2.55), total bilirubin 13 umol/l, direct bilirubin 7.5 (0-3.0), GGT 175 u/l, K 3.2 mmol/l (3.5- 5.1) and albumin 27 g/l (34-50).
Investigation also showed serum calcium range from 2.85-3.0 mmol/L (2.13-2.63), phosphorus 0.7 mmol/L (0.8, 1.4) and magnesium 0.6 mmol/L (0.74, 1). The mean parathyroid hormone level (PTH) was above 30.4 pmol/L (1.69-6.9) or 198.5 pg/ml (15-65), which confirmed our suspicion of hyperparathyroidism. In addition the calcium to creatinine ratio was increased to 0.11 (normal limit < 0.06). Abdominal ultrasound showed multiple right renal calculi and mild hydronephrosis (see Figure 2); and neck ultrasound showed a low echogenic mass (1.3x1.5x3.3 cm) that intensified suspicion of a right inferior parathyroid adenoma (see Figure 3).
 Figure 2: Abdominal ultrasound showing right renal stone
Figure 2: Abdominal ultrasound showing right renal stone
 Figure 3: Neck ultrasound showing enlarged right lower parathyroid lobe
Figure 3: Neck ultrasound showing enlarged right lower parathyroid lobe
Chest x-ray showed mild cardiomegaly with both lung fields clear, while ECG was normal and cardiac stress test showed no significant cardiac lesion, whereas 2D echo with color Doppler showed concentric hypertrophy of the left ventricle with normal function (see Figure 4).
 Figure 4: Echo showing concentric left ventricular hypertrophy
Figure 4: Echo showing concentric left ventricular hypertrophy
Parathyroid scintigraphy was suggestive of parathyroid adenoma of right inferior gland, and bone DXA result showed osteopenia with increased risk of major osteoporotic fracture to 5.7%.
Finally, the case was referred to a surgeon and a right inferior nodular mass measuring 3.2x1x0.4 cm was removed. Microscopic examination revealed features consistent with parathyroid adenoma (the lesion had a slender capsule all around and was composed of trabeculae of cells separated by vascular sinusoids with foci of hemorrhage and cystic change). The cells were large, polygonal with vesicular nuclei having small nucleoli and abundant finely granularto- clear cytoplasm. There was no significant pleomorphism, mitosis, capsular or vascular invasion.
The patient was discharged from the hospital three days postoperatively and her follow-up investigation (six months later) showed parathyroid, calcium, magnesium and phosphate levels had returned to normal. Also, the patient had shown improvement of all her symptoms of hypercalcemia.
Primary hyperparathyroidism is the most common cause of hypercalcemia in primary care. Family physicians should be alert to the diagnosis of primary hyperparathyroidism. Symptomatic hypercalcemia occurs with longstanding elevated levels of PTH6. This patient showed renal manifestation of nephrolithiasis, but no nephrocalcinosis, polyuria, or renal insufficiency7. Although our patient showed left ventricular hypertrophy, other cardiac manifestations were not present (conduction abnormalities, endothelial dysfunction, and shortened QT intervals). Parathyroidectomy is the appropriate treatment in symptomatic hyperparathyroidism, and the patient’s clinical and biochemical status improved dramatically.
In most patients primary hyperparathyroidism is associated with hypercalcemia but the reverse is not the case. Screening for serum calcium for any patient above 50 years of age is essential to diagnose missed primary hyperparathyroidism. Surgery offers the only opportunity for permanent cure of primary hyperparathyroidism.