
Journal of the Bahrain Medical Society
Year 2018, Volume 30, Issue 2, Pages 17-24
https://doi.org/10.26715/jbms.2_18072018Ahmed Malallah Al Ansari1*, Haitham Ali Jahrami1, 2, Rami Ghazi Hafedh3, Isa Mohammed Sharif1
1College of Medicine and Medical Sciences, Arabian Gulf University, Road 2904, Building 293, Manama 329, Kingdom of Bahrain.
2Psychiatric Hospital, Ministry of Health, Building 1228, Road 4025, Juffair 340, Kingdom of Bahrain.
3Mental Health Hospital, Jeddah, Kingdom of Saudi Arabia.
*Corresponding author:
Ahmed Malallah Al Ansari, Family Practice Residency Program, Ministry of Health - Kingdom of Bahrain. P.O. Box 42. Tel: (+973) 17263597, Fax: (+973) 17251104, Email: AHammad1@health.gov.bh
Received date: May 11, 2018; Accepted date: July 18, 2018; Published date: September 21, 2018

Background and objectives: The impact of caring for a child with autism has been observed among mothers of children with autism spectrum disorders (ASDs) in western countries, however, there is a scarcity of data in the Arab countries. The study aimed to compare the mental health, quality of life (QOL), and general functioning of mothers of young children and adolescents with autism.
Methods: This cross-sectional study, including 60 mothers of children with ASD was conducted in the Child Psychiatry Unit of Psychiatric Hospital, Bahrain. Data regarding the mothers’ demographic characteristics, general health, QOL, and functioning were collected through interviews. The children were consecutively diagnosed and followed-up at the Psychiatric Hospital, Bahrain. The differences between the mothers of young children and the mothers of adolescent children with ASD were compared.
Results: The mothers of both the groups reported elevated physical health complaints, mental health symptomatology, and decreased experience of QOL. Mothers of young children with ASD reported depressive symptoms, less physical illness, and fewer comorbidities in the young children with ASD, when compared to mothers of adolescents who reported anxiety symptoms, more physical illness, and better QOL-related psychological wellbeing and environmental factors.
Conclusion: The issue of mothers’ health requires attention and should be addressed in the management of children with ASD, especially in clinical practice with interventions specific to the child’s age.
Keywords: Autism spectrum disorders, mothers, stress, quality of life, health
Autism Spectrum Disorders (ASD) are neurodevelopmental disorders characterized by impairment in verbal and nonverbal communication, socialization, living independently, repetitive movements, and restricted activities.1 The recent combined estimated prevalence of ASD is 4.6 per 1,000 or one in 68 children aged 8 years.2 In the Arabian Gulf countries the prevalence rates reported in Oman, United Arab Emirates, and Bahrain are 1.4 per 10,000, 29 per 10,000, and 4.3 per 10,000 children.3 ASD has a long-lasting negative impact on the individual as well as the family’s Quality of Life (QOL).4 According to literature, parents of a child with ASD have more psychiatric disorders than parents of children with typical development.5 Specifically, mothers of children with ASD are three times more prone to high depression scores than mothers of unaffected children.6 Furthermore, 50% of the parents of children with ASD have clinical depression and 41% have anxiety disorders.6, 7
Parents of children with ASD presented with more symptoms of stress and difficulties in social relationships and performing physical activities. The perception of these parents regarding their QOL was lower than other parents.8 The effect of having a child with ASD on parents extends to include financial and career impacts.9–11 The children with ASD level of social skill is a determinant of his/ her mother’s stress level.12 Consequently, depressed mothers might not be able to deal effectively with their children’s problems and challenges, thus raising questions regarding the unmet mental health needs of parents of children with ASD.13
In our region, few studies reported the impact of having a child with ASD on the physical and mental health of mothers. In Oman, a study reported that parents are at 1.8 times higher risk of depression, anxiety, and stress than parents of a normal child.14 In Qatar, a study that examined the concerns of caregivers towards their children found pessimism of caregivers about the future of their children and they had a major concern regarding the services provided to their children.13 Another study in Qatar analyzed the QOL of caregivers of children with ASD and found no difference against caregivers of healthy children.15
This study is part of a larger ongoing unpublished study that measures the impact of caring for a child with ASD on the mothers’ health. In this study, we are comparing the impact of having a child with ASD on mothers’ health; the different child age groups are: early childhood ≤ 6 years and adolescence ≥ 12 years. Both age groups received similar interventions that were standardized by standard protocol.
This prospective cross-sectional study was conducted in conjunction with the Bahrain Association of Intellectual Disability and Autism (BAIDA) between September and December 2016.
The Association provides services through 2 main centers: Al-Wafa Center—enrolling children aged 2–11 years with ASD; Al-Rashid Center—enrolling adolescents aged 12–18 years with ASD.
Mothers of all children aged ≤ 6 years attending Al-Wafa Center for Autism (group I, n = 30) and mothers of all adolescents aged ≥ 12 years attending Al-Rashad Center for Autism (group II, n = 30) were enrolled in the study. Inclusion criteria were that all cases were to be diagnosed according to Diagnostic and statistical manual of mental disorders-IV (DSM-IV-TR) criteria,16 regularly attend their rehabilitation center, and willing to participate in the research. Exclusion criteria were the unavailability of the mother for interview due to death or long-term travel. The participant was recruited as a convenient sample. Participants for both groups (centers) were accepted in their respective center using a similar set of criteria. Participants from Al-Wafa Center (group I) were transferred to Al-Rashad Center according to their age. All the mothers from groups I and II participated in the study. Written informed consent was sought from each participant prior to the interview.
Mothers in group I and II were interviewed face to face by one of the authors using data collection sheet in the Arabic language designed for the study. Data collection focused on obtaining information regarding the presence of physical and mental difficulties, legal, mental, or (psychiatric) problems, and need for extra help for raising children with ASD.
In addition, mothers were asked to complete two other forms, including the General Health Questionnaire-28 items (GHQ-28) and the World Health Organization Quality of Life, Brief Version (WHOQOL-BREF)17. These forms were selfadministered and were to be completed within 15–20 minutes.17 At the end of the interview, two authors completed the Global Assessment of Function (GAF)16 form for each participant. All the measures used in our research were available and standardized in the Arabic language.
The WHOQOL-BREF instrument comprises of 26 items, which measure the following broad domains: physical health, psychological health, social relationships, and environment factors. The WHOQOL-BREF is a shorter version of the original instrument, which is more convenient for use and the instrument can be self-administered on a 5-point Likert scale for the 26 questions. It has sound psychometrics with an internal consistency— Cronbach’s alpha—for the overall scale of 0.89 (range: 0.74–0.77 for individual domains). All values were above 0.70, which demonstrated adequate internal consistency.17
The GHQ-28 was developed as a screening tool to detect those likely to have or to be at risk of developing psychiatric disorders. The GHQ- 28 is a 28-item measure of emotional distress in medical settings. It is divided into four subscales based on different symptoms: somatic symptoms (items 1–7); anxiety/insomnia (items 8–14); social dysfunction (items 15–21), and severe depression (items 22–28). Numerous studies have investigated reliability and validity of the GHQ-28 in various clinical populations. Test-retest reliability has been reported to be high (0.78–0 0.9) and inter-rater and intra-rater reliability and internal consistency were all excellent (Cronbach’s α: 0.9–0.95).18
The GAF is a numeric scale used by mental health clinicians and physicians to rate subjectively the social, occupational, and psychological functioning of an individual; for example, how well one is meeting various problems-in-living. Scores range from 1 (severely impaired) to 100 (extremely high functioning). The GAF is a brief measurement of the assessment of general daily functioning at work and activities of daily routine and the leisure time.
Social class was constructed using modified Hollingshead and Redlich scale for a social class designed on a 5-level Likert type scale, level one being high and level five low. The level depended on the children’s father’s education level and job.19
Neither the mothers nor the children were physically examined. Data regarding children’s cognitive function were not obtained either at baseline initial diagnosis or at the time of the study. Participation in the study was voluntary and did not affect the services provided by the center for both the child and the mother. Ethical approval was obtained from the Research and Ethics Committee, Ministry of Health, Kingdom of Bahrain.
Data were entered in SPSS 22. Descriptive statistics were summarized for the demographic data and outcome measures. The mean and standard deviation (SD) were reported for continuous variables, and count and percentage were reported for categorical variables. Pearson Chi square test or Fisher’s exact test and independent samples t-test were used to investigate the differences between the two groups.
Table 1 provides summary of the sociodemographic characteristics of the study participants, and comparison between groups I and II using appropriate statistical tests. The mothers in both the groups were similar in terms of sociodemographic characteristics.
Table 1: Differences in sociodemographic characteristics of the study participants*
*Please refer the pdf.
In Group I the mean age of the children was 4.9 ± 1.0 years; and mean age of the children at diagnosis was 2.5 ± 2.8 years. The mothers were young with a mean age of 33.6 ± 6.5 years; majority (96.7%) of mothers were married and around twothirds of them were university graduates.
In Group II the mean age of the children was 17.7 ± 6.1 years; and mean age of the children at diagnosis was 4.2 ± 2.2 years. The mothers were middle aged with a mean age of 44.9 ± 7.9 years; majority (86.7%) of mothers were married and around half of them were university graduates. The details of the mothers’ chronic medical illness, psychiatric illness, and family and legal issues for both the groups are shown in Table 1.
The results of GHQ-28, WHOQOL-BREF, and GAF of all the mothers are shown in Table 2. Based on the scores revealed by GHQ-28, the scores of somatic symptoms (2.0 ± 1.9 vs. 1.7 ± 2.1) a2nd anxiety/insomnia (2.7 ± 2.3 vs. 2.7 ± 2.4) are similar among mothers in both the groups I and II. Furthermore, the scores of severe depression (1.4 ± 1.6 vs. 1.2 ± 1.44) and social dysfunction (1.6 ± 1.6 vs. 1.16 ± 1.9) were higher in mothers in group I when compared to mothers group II (1.4 ± 1.6 vs. 1.2 ± 1.44).
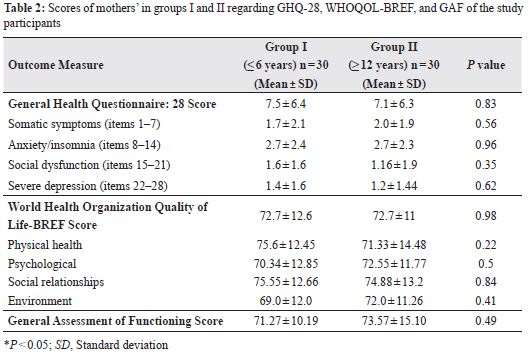
QOL was similar in both the groups with a mean score of 72.17 ± 12.6 vs. 72.7 ± 11 in group I and II, respectively. Subscale analysis of WHOQOLBREF revealed that mothers of young children were better in physical health while mothers with adolescents scored better in psychological wellbeing and environmental factors, although they were not significant.
Examination of the GAF scores revealed that both the groups scored within the category 71–80, which interprets that the symptoms exist and are transient and expectable reactions to psychosocial stressors; no more than slight impairment in social, occupational, or school functioning.
The sociodemographic data revealed that mothers in groups I and II were similar in marital status, education, number of children, mother’s work status, the presence of legal issues, and consanguinity rate. However, mothers in both the groups were significantly different with regard to mean age, socioeconomic status, and child comorbidity of ASD with intellectual disability.
In addition, many mothers in group II were retired— indicative of previous working status, prevalence of mental and physical illnesses, and family-related child behavior problems. This could be partly due to the related difference in age of mothers in both the groups. The approximate age of mothers in group II was late forties and early fifties, an age at which several women in Bahrain consider retirement and tend to develop age-related physical problems. According to literature, some children with ASD develop more behavioral problems and seizure disorders during their adolescence,20 which increases the stress on family dynamics and can adversely affect marital relationships leading to family issues.21
The study justifies the fact that the health of mothers of children with ASD is not addressed adequately, which is similar to the literature, particularly, in the Eastern Mediterranean region. The relationship of child age with the degree of impact on the mother’s health was not examined by previous researchers, i.e. what is the general functioning of the mothers of children with ASD at different times after the initial diagnosis of ASD and how they are coping with new challenges of the child’s advancing age.
An incidental observation was that there is a decrease in mean age at diagnosis of ADHD over the 10 years period (1981–2011) from 4.5 years to 2.8 years. This indicates an increase in public and professional interest and awareness about the disorder. This was supported by the previous study in Bahrain where the percent of the referred cases to the main child psychiatric clinic increased from 1.54% to 13.3% in 1981–2011, respectively.22
The impact of caring for a child with ASD on the health-related QOL of the mothers is not completely understood. However, parents of children with ASD had lower health-related QOL scores than the general population.23 Khanna et al. reported that the extent of behavioral problems and the presence of social support influence the caregiver’s physical health-related QOL, whereas the level and functional impairment, social support, and use of maladaptive coping strategy effects the mental health-related QOL.23
The difference in the socioeconomic status of the two groups is related to the income as both groups were identical in education level. Older aged mothers in group II worked for a longer period and/ or received retirement pension much more than the younger mothers in group I. Mothers in group I received significant extra help from their families in childcare, perhaps because these mothers are still coming to terms with the diagnosis of autism of their child.
A previous study evaluated the impact of selfnarratives of motherhood for mothers of children with ASD and observed a baseline difference in mothers with young children (2–3 years) and mothers with older children (9–12 years) with higher scores in different scales in mothers with older children.24
Prevalence of depression among mothers group I can be interpreted as a loss of a dream child, who is now labeled as disabled. The depression is substituted by worries and anxieties as children grow older. It was expected that the QOL physical health would be better among mothers of young children due to the age factor, shorter duration of stress exposure, and less severe disability of their children. The scores of GAF as an objective measure of functioning showed high concordance with the results of GHQ-28, which is suggestive of the fact that level of functioning is strongly associated with mental health status.
Although mothers in both the groups scored in measures of GAF, GHQ-28, and WHOQOL-BFEF, the observed differences in subtests merit further discussion. For example, anxiety symptoms were more pronounced among mothers of adolescents with ASD using GHQ-28. These observations could be due to the fact that as the child grows older, mother’s worries about future opportunities for work, marriage, and independent living increase. In contrast, mothers of younger children with ASD are still optimistic about the future outcome of their children. In addition, most rehabilitation centers provide regular rehabilitation services up to 18 years of age only. Hence, the demands placed by a growing child with this disability has a major effect on mothers’ coping mechanism, which is in concordance with studies conducted in Pakistan21 and China6. Overall, the findings of this study partly confirmed our initial hypothesis that the impact on mother’s health and quality of life varied based on the child’s age and degree of difficulties and challenges faced by mothers. However, the results fail to prove the hypothesis that the impact was greater in mothers of younger children compared to mothers of an adolescents with ASD.
The major strength of our research is the use of three validated measures to comprehensively assess the physical health, mental health, and QOL of mothers of children with ASD in one single sample. Our results also add further information to the subject in the region.
The limitations include the lack of information on the magnitude of disability among children with ASD, small sample size, selection bias, and generalizability. Furthermore, some of the findings are reflective of mothers’ perceptions and were measured only once by using a cross-sectional study design.
Mothers of adolescents with ASD should be educated and counseled regarding future outcomes and resources available to reduce their qualms. Simultaneously, researchers are encouraged to evaluate the effectiveness of counseling programs for mothers through long-term follow-up with studies on mothers’ QOL and general health.
Mothers of young children and adolescents with ASD did not show substantial differences in mental, physical health, and QOL measures. However, mothers of young children with ASD had more depressive symptoms and better physical health. Mothers of adolescents with ASD had more anxiety symptoms and poor physical health. The total score of QOL in both groups was identical, however, mothers of young children had better physical health and mothers of adolescents had a better environment and psychological well-being. It is important to determine the factors associated with advancing age of mothers and severity of symptoms in children with ASD, which are crucial in assessing the impact of having a child with ASD on mothers’ health across childhood and adolescence.
The authors of the study have no conflict of interest to declare.